Macrolide Arrhythmia Risk Calculator
When you take an antibiotic for a stubborn infection, you expect relief-not a hidden risk to your heart. But for some macrolide antibiotics, that risk is real. Macrolides like azithromycin, clarithromycin, and erythromycin are commonly prescribed for pneumonia, bronchitis, and sinus infections. Yet, behind their effectiveness lies a quiet danger: they can disrupt the heart’s electrical rhythm and trigger a life-threatening arrhythmia called Torsades de pointes (TdP). This isn’t theoretical. It’s documented, measured, and tracked by the FDA, the American Heart Association, and major medical journals. The good news? For most healthy people, the risk is tiny. The problem? It spikes dramatically when you have even one other risk factor. And that’s where things get dangerous.
How Macrolides Disrupt Your Heart’s Timing
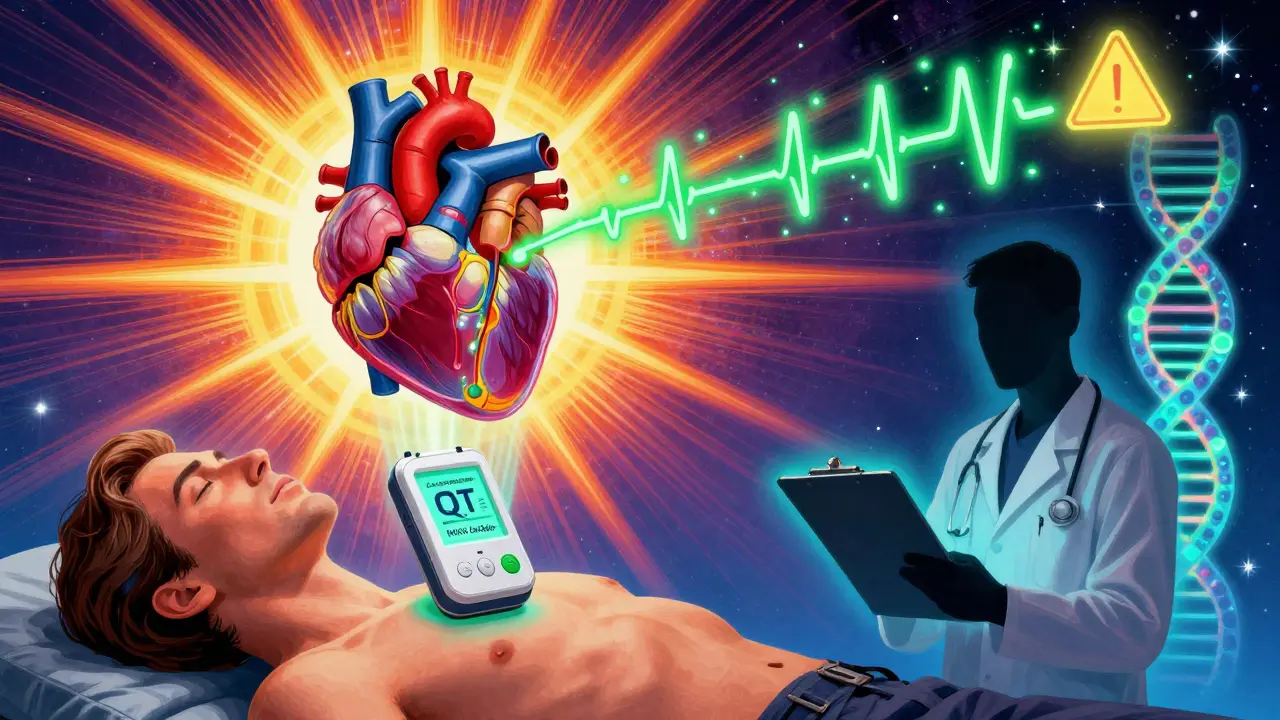
Your heart beats because of a precise sequence of electrical signals. One key moment is repolarization-the phase when heart cells reset after contracting. This reset is controlled by potassium channels, especially the hERG channel that carries the rapid potassium current (Ikr). Macrolide antibiotics bind directly to this channel, blocking the flow of potassium out of heart cells. That delay means the heart takes longer to reset. On an ECG, that shows up as a longer QT interval. A prolonged QT isn’t just a number-it’s a warning sign. When the interval stretches too far, the heart becomes electrically unstable. This can spark early beats called afterdepolarizations, which cascade into TdP: a chaotic, fast rhythm that can lead to sudden cardiac arrest.
Not all macrolides are equal in this risk. Studies show that clarithromycin is the strongest blocker of Ikr channels, followed closely by roxithromycin and then erythromycin. Azithromycin blocks the channel less potently, which is why it was long considered the safest. But here’s the catch: even weak blockers can be dangerous when combined with other risks. In 2012, a landmark study of over 1.3 million patients found that azithromycin use led to 2.85 extra cardiovascular deaths per 1,000 courses compared to amoxicillin-mostly within the first five days of treatment. That’s not a huge number overall, but for someone with a weak heart or low potassium, it’s enough to tip the balance.
The Real Danger: When Risk Factors Stack Up
Most people who take macrolides never have a problem. But if you have even one of these six risk factors, your chance of developing TdP jumps significantly:
- Female sex: 68% of documented TdP cases occur in women. Why? Hormonal differences affect potassium channel function.
- Age over 65: The heart’s electrical system slows naturally with age. Older adults have less “repolarization reserve”-a buffer that protects against arrhythmias.
- Baseline QTc over 450 ms: If your ECG already shows a prolonged QT, adding a macrolide can push it past the danger zone.
- Other QT-prolonging drugs: Taking azithromycin with a statin, antidepressant, or antifungal? That’s additive risk. Each extra drug increases danger by about 1.8 times.
- Low potassium or magnesium: Hypokalemia increases TdP risk 3.1-fold. This is why severe vomiting or diuretics are red flags.
- Structural heart disease: Heart failure raises risk by 5.3 times. The damaged heart tissue is more prone to electrical chaos.
Here’s what’s scary: many people don’t know they have a hidden risk. About 5-20% of those who develop TdP after taking a macrolide have an undiagnosed inherited long QT syndrome. They’ve never had symptoms. Their ECG looked fine. Then came the antibiotic-and their heart went haywire.
Clarithromycin vs. Azithromycin: The Risk Difference You Need to Know
It’s not just about how strong the drug is at blocking potassium channels. Clarithromycin has a second dangerous trick: it blocks the liver enzyme CYP3A4. This enzyme breaks down many other medications. When it’s inhibited, those drugs build up in your blood. So if you’re on a statin, a blood thinner, or even a common antifungal, clarithromycin can turn them into hidden heart poisons. That’s why the FDA requires a black box warning on clarithromycin labels.
Azithromycin barely touches CYP3A4. That’s why it’s prescribed far more often-about 65% of all macrolide prescriptions in the U.S. But that doesn’t make it safe. A 2023 study in Frontiers in Cardiovascular Medicine showed that azithromycin’s real-world risk is higher than lab tests suggest. During the pandemic, when azithromycin was combined with hydroxychloroquine (another QT-prolonging drug), QTc increased by an average of 26.2 milliseconds. That’s enough to push many patients over the danger line. The FDA’s own data from 2001 showed 10 cardiac events per 10 million azithromycin prescriptions. Sounds rare? Multiply that by the 50 million courses prescribed annually in the U.S., and you’re talking about dozens of preventable cases each year.
What Doctors Should Do-And What They Often Miss
Guidelines from the American College of Cardiology and the Infectious Diseases Society of America are clear: check an ECG before prescribing macrolides if the patient has two or more risk factors. But in practice? Most doctors don’t. Why? Because they think, “It’s just a common infection.” They don’t ask about family history of sudden death. They don’t check recent labs for potassium. They don’t review every medication the patient is taking.
Here’s what should happen:
- If QTc is over 470 ms in men or 480 ms in women, avoid macrolides entirely.
- If QTc increases by more than 60 ms from baseline during treatment, stop the drug.
- If the patient has heart failure, a history of arrhythmias, or is on multiple QT-prolonging drugs, choose an alternative antibiotic like amoxicillin or doxycycline.
- For patients with unexplained fainting or family history of sudden cardiac death under age 50, assume they may have hidden long QT syndrome-don’t give macrolides.
Even if the patient is young and healthy, if they’re on a diuretic for high blood pressure or taking an antihistamine like cetirizine, the risk isn’t zero. The 2025 NIH review calls this the “repolarization reserve” concept: everyone has some buffer. But if you’ve already used up that buffer with other drugs, genetics, or illness, the macrolide is the last straw.
What’s Changing Now-And What’s Coming
Things are starting to change. In 2023, the FDA approved the CardioCare QT Monitor, a handheld ECG device that gives accurate QTc readings in under 30 seconds. Emergency rooms and urgent care clinics are starting to use it before prescribing azithromycin. In 2024, the Macrolide Arrhythmia Risk Calculator (MARC) launched. It takes 12 inputs-age, sex, meds, labs, heart history-and predicts your personal TdP risk with 89% accuracy. It’s not in every doctor’s office yet, but it’s a sign of where we’re headed.
Research is also looking at new macrolides. Solithromycin was designed to be safer-it blocked 78% less Ikr than clarithromycin in trials. But it was pulled from development in 2022 because of liver toxicity. Now, scientists are testing drugs like nicorandil, a potassium channel opener, to counteract QT prolongation. Early results show it can shorten QTc by over 30 ms in patients on macrolides. That could be a game-changer for high-risk patients who absolutely need these antibiotics.
And then there’s genetics. Preliminary data suggests 15% of people carry a gene variant that makes their hERG channels extra sensitive to macrolides. If you have this variant, even a normal dose can trigger TdP. We’re not testing for it yet-but we will be soon.
What You Should Do
If you’re prescribed a macrolide:
- Ask: “Do I have any risk factors for heart rhythm problems?”
- Know your medications. List every pill you take-including over-the-counter ones.
- If you’ve had fainting spells, irregular heartbeats, or a family member who died suddenly before age 50, tell your doctor.
- If you’re on diuretics, have heart failure, or are over 65, ask if an alternative antibiotic is available.
- If you’re given azithromycin, watch for dizziness, palpitations, or fainting in the first few days. Call your doctor immediately.
Macrolides save lives. But they’re not risk-free. The key isn’t avoiding them entirely-it’s using them wisely. For the majority, they’re safe. For a small but vulnerable group, they can be deadly. The difference? Awareness. Knowledge. A simple ECG. A few questions. That’s all it takes to prevent a tragedy.




Prateek Nalwaya
February 15, 2026 AT 12:21