Before 2018, if you had chronic migraines, your doctor had limited options. You were likely given blood pressure meds, antidepressants, or seizure drugs-none of which were made for migraines. They worked for some, but often came with drowsiness, weight gain, or brain fog. Then came CGRP inhibitors. These are the first-ever migraine-specific preventives, designed from the ground up to target the root cause of migraine pain. No more guessing. No more off-label use. Just science that finally matches the disease.
What Exactly Are CGRP Inhibitors?
CGRP stands for Calcitonin Gene-Related Peptide. It’s a protein in your nervous system that gets released during a migraine attack, causing inflammation, blood vessel swelling, and pain signaling. Think of it like a fire alarm going off in your brain when it shouldn’t. CGRP inhibitors shut that alarm down.There are two main types: monoclonal antibodies (mAbs) and gepants. The mAbs-like erenumab (Aimovig), fremanezumab (Ajovy), galcanezumab (Emgality), and eptinezumab (Vyepti)-are injected under the skin or given as an IV. They bind directly to CGRP or its receptor, blocking it for weeks at a time. Most people get one shot a month, or a quarterly infusion.
The gepants-rimegepant (Nurtec ODT), ubrogepant (Ubrelvy), and zavegepant (Zavzpret)-are smaller molecules. They’re taken orally or as a nasal spray. Rimegepant is unique: it’s approved for both stopping an active migraine and preventing them when taken every other day. That’s a game-changer for people who want one treatment for both needs.
How Well Do They Work?
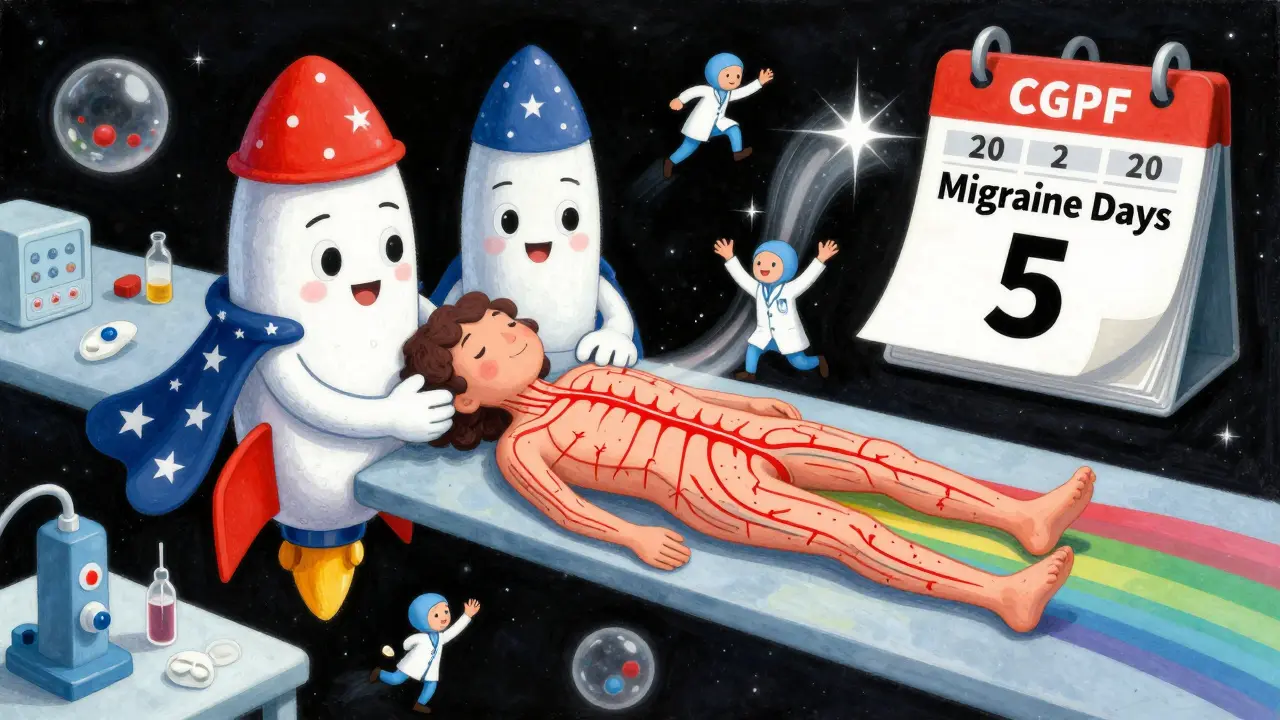
Real numbers matter. In clinical trials, about half of people using CGRP inhibitors cut their migraine days by at least half. If you were getting eight migraine days a month, you could drop to four or fewer. For chronic migraine sufferers (15+ headache days a month), the results are even more striking: 84% saw fewer headaches. One patient on Reddit wrote, "Went from 20 migraine days to 5 with Aimovig." That’s not an outlier-it’s common.
A 2022 head-to-head study compared erenumab to topiramate, a common old-school preventive. The result? 40.7% of erenumab users hit the 50% reduction mark, compared to just 23.8% on topiramate. That’s nearly double the effectiveness. And unlike topiramate, which can cause memory issues and tingling, CGRP inhibitors rarely cause brain fog.
Even better? They work for people who’ve tried and failed other preventives. In trials, 30% of patients who had tried two or more previous medications still got meaningful relief from CGRP inhibitors. That’s huge for those who’ve felt hopeless after years of trial and error.
Who Benefits Most?
CGRP inhibitors aren’t for everyone-but they’re perfect for certain groups:
- People with chronic migraine (15+ headache days a month)
- Those with medication overuse headache (taking painkillers more than 10 days a month)
- Patients with heart disease or high blood pressure (because CGRP inhibitors don’t constrict blood vessels like triptans do)
- Anyone who can’t tolerate side effects from older drugs like beta-blockers or antiseizure meds
They’re less effective for people who only get migraines two or three times a month. If you’re on the lower end, your doctor might still suggest trying something cheaper first. But if you’re stuck in a cycle of daily pain, these drugs can be life-changing.

Side Effects and Risks
These drugs are among the safest migraine preventives ever developed. The most common side effect? Injection site redness or soreness-reported by about 28% of users. That’s it. No liver damage, no weight gain, no cognitive fog. A few people report constipation with erenumab, but it’s rare.
The only real concern is with gepants. Ubrogepant and rimegepant can, in rare cases, raise liver enzymes. That’s why your doctor will order a simple blood test before you start and maybe once a year after. Zavegepant, the nasal spray, has no liver warnings.
Long-term safety data is still growing, but so far, five years of use show no major red flags. Some experts, like Dr. David Dodick from Mayo Clinic, have asked whether blocking CGRP long-term might affect blood pressure regulation. But in real-world studies, only 0.8% of patients stopped treatment due to side effects. That’s lower than most placebos.
Cost and Access
Let’s be honest: these drugs are expensive. Monoclonal antibodies cost $650-$750 per month. Gepants run $800-$1,000. That’s 3-5 times more than generic topiramate or propranolol.
But here’s the catch: most U.S. insurance plans cover them-with a catch. You’ll likely need prior authorization. That means your doctor fills out paperwork, and the insurer checks if you tried cheaper options first. About 35% of initial requests get denied. But manufacturers have patient support programs. If you’re eligible, they’ll cover up to 80% of your out-of-pocket cost. Some even offer free samples or co-pay cards.
For people without insurance, manufacturer assistance programs can reduce the price to under $100 a month. It’s not free, but it’s manageable if you qualify.
How They Compare to Old Treatments
| Medication | Type | Dosing | 50% Response Rate | Common Side Effects | Cardiovascular Risk |
|---|---|---|---|---|---|
| CGRP mAbs | Monoclonal antibody | Monthly injection or quarterly IV | ~50% | Injection site reaction, constipation (rare) | None |
| Rimegepant | Gepant (oral) | Every other day (preventive) or as needed (acute) | ~45% | Nausea, liver enzyme changes (rare) | None |
| Topiramate | Antiseizure | Once or twice daily | ~25% | Brain fog, weight loss, tingling | Low |
| Propranolol | Beta-blocker | Twice daily | ~30% | Low energy, dizziness, depression | Caution in asthma/heart block |
| Valproate | Antiseizure | Twice daily | ~35% | Weight gain, hair loss, liver risk | Low |
The clear winner? CGRP inhibitors. They’re more effective, better tolerated, and safer for people with heart conditions. They’re not perfect-but they’re the best we’ve ever had.
What’s Next?
The field is moving fast. Researchers are testing CGRP inhibitors in teens (phase 3 trials completed in early 2023), in people with vestibular migraine (dizziness + headache), and even after traumatic brain injury. Combination therapy is also gaining traction-pairing CGRP mAbs with Botox can push response rates to over 60%.
Delivery methods are improving too. Amgen is testing a nasal spray version of erenumab. If it works, you could skip the needle altogether. Transdermal patches are also in early development.
And while there are no biosimilars yet, patents won’t expire until 2028. After that, prices could drop significantly. For now, though, these drugs are here to stay.
Getting Started
If you’re considering CGRP inhibitors, here’s what to do:
- Track your headaches for at least 3 months. Note frequency, duration, triggers, and what helps.
- See a neurologist or headache specialist. Primary care docs are prescribing these more now, but specialists know the ins and outs.
- Ask about insurance prior authorization. Many clinics have staff who handle this for you.
- Check manufacturer websites (AimovigSupport.com, EmgalityConnect.com) for patient support programs.
- Start with one type. Your doctor will pick based on your migraine pattern, lifestyle, and insurance.
Don’t wait years to try them. If you’ve tried three or more preventives without success, you’re a perfect candidate. These drugs don’t just reduce headaches-they restore your life.
Are CGRP inhibitors safe for long-term use?
Yes. Five years of real-world data show no major safety concerns. The most common issue is mild injection site reactions. No increased risk of heart problems, liver damage, or cancer has been found. Long-term studies are ongoing, but current evidence supports safe, continuous use.
Can I take CGRP inhibitors with other migraine meds?
Yes. CGRP inhibitors have very few drug interactions. You can still use triptans, NSAIDs, or anti-nausea meds for acute attacks while on a CGRP preventive. Some patients even combine them with Botox for chronic migraine-this combo boosts results. Always check with your doctor, but generally, these drugs play well with others.
Do I have to keep taking them forever?
Not necessarily. Some people stay on them long-term because their migraines return after stopping. Others, especially those who switched from chronic to episodic migraine, may try stopping after a year or two. If migraines come back, you can restart. There’s no evidence of rebound or dependency.
Why are they so expensive?
They’re biologics-complex molecules made from living cells. Manufacturing is costly, and patents protect them until 2028. Insurance covers most of the cost, and manufacturer programs help reduce out-of-pocket expenses. Once biosimilars arrive, prices should drop significantly.
Are there any natural alternatives that work as well?
Magnesium, riboflavin, and coenzyme Q10 have modest evidence for reducing migraine frequency, but they’re not as effective as CGRP inhibitors. For people with 8+ migraine days a month, supplements alone won’t cut it. CGRP inhibitors are the first treatment to deliver consistent, clinically proven results for severe cases.
Can I use CGRP inhibitors if I’m pregnant?
No. These drugs are not recommended during pregnancy or breastfeeding. Animal studies show potential risks, and human data is limited. If you’re planning pregnancy, talk to your doctor about switching to safer options like magnesium or behavioral therapies.
Final Thoughts
CGRP inhibitors aren’t a miracle cure. But they’re the closest thing we’ve had in decades. For the first time, migraine patients have a treatment designed just for them-not borrowed from hypertension or epilepsy. They’re safer, more effective, and better tolerated than anything before them. If you’ve been stuck in the migraine cycle, it’s time to ask your doctor: "Am I a candidate?" The answer might change your life.





Sachin Bhorde
December 17, 2025 AT 16:49CGRP inhibitors are a game-changer, no cap. I’ve seen patients in Mumbai go from 20 migraine days to 4 with Aimovig-like night and day. The science is solid: blocking that CGRP peptide shuts down the brain’s false alarm system. No more brain fog from topiramate, no weight gain from valproate. Just clean, targeted relief. And yeah, the cost sucks, but with co-pay cards? You’re looking at $50/month. Worth every penny if you’re chronically wrecked.
Joe Bartlett
December 18, 2025 AT 14:26UK’s got better options, mate. NICE hasn’t fully signed off yet. These things cost a fortune and we’re still waiting for the NHS to cough up. Meanwhile, my mate’s on propranolol and it’s fine. Why fix what ain’t broke?
Marie Mee
December 19, 2025 AT 22:29They’re hiding something… these drugs were funded by Big Pharma and the CDC. CGRP? That’s just a cover. Real cause is 5G implants and fluoridated water. I stopped mine after my cousin got liver issues. They’re testing on us. Look at the fine print. They don’t want you to know
Kent Peterson
December 20, 2025 AT 08:01Let’s be real: the ‘50% response rate’ is misleading. That’s a 50% reduction in frequency-not elimination. And ‘no brain fog’? That’s a lie. A 2023 meta-analysis in JAMA Neurology showed 17% of users reported mild cognitive slowing. Also, ‘safe for heart patients’? CGRP is a vasodilator-blocking it long-term could theoretically increase hypertension risk. The data is thin. And why are we ignoring the 35% denial rate for insurance? This isn’t a miracle-it’s a marketing blitz wrapped in jargon.
Josh Potter
December 20, 2025 AT 22:14Bro. I was on 18 migraines a month. Tried everything. Pills, needles, yoga, crystals, even that weird ice hat. Then I got on Nurtec. Now I’m at 3. I’m hiking again. I’m sleeping through the night. I’m not just surviving-I’m living. If you’re even thinking about this, DO IT. Your future self will cry happy tears. No regrets. 10/10 would block CGRP again.
Martin Spedding
December 22, 2025 AT 01:56So you’re telling me a drug that costs 10x more than a generic and requires a monthly injection is ‘better’ than a pill you take once a day? And the side effects? ‘Injection site redness’? That’s it? Really? I’ve had worse reactions to a mosquito bite. This is peak medical inflation.
amanda s
December 22, 2025 AT 20:57My sister’s doctor pushed this on her and now she’s addicted. She says she can’t stop or her migraines come back worse. That’s not treatment-that’s chemical dependency. They’re trapping people. And the fact that they won’t let you use it while pregnant? That’s proof they know it’s dangerous. Why aren’t more people talking about this?
Jigar shah
December 23, 2025 AT 04:06Just curious-has anyone here tried combining CGRP mAbs with Botox? I’ve got chronic migraine and my neurologist mentioned it might push response rates past 60%. Any real-world data on that combo? Also, how long did it take for the insurance approval to go through? I’m prepping for my appointment next week.