Most people with fatty liver don’t feel sick. No pain. No jaundice. No obvious warning signs. That’s why so many don’t find out until their liver is already damaged - sometimes severely. The terms NAFLD and NASH get thrown around a lot, but they’re not the same thing. One is a quiet buildup of fat. The other is active liver injury that can lead to scarring, cirrhosis, or even liver cancer. Understanding the difference isn’t just medical jargon - it’s the line between watching and waiting, and taking real action.
What’s Really Going On in Your Liver?
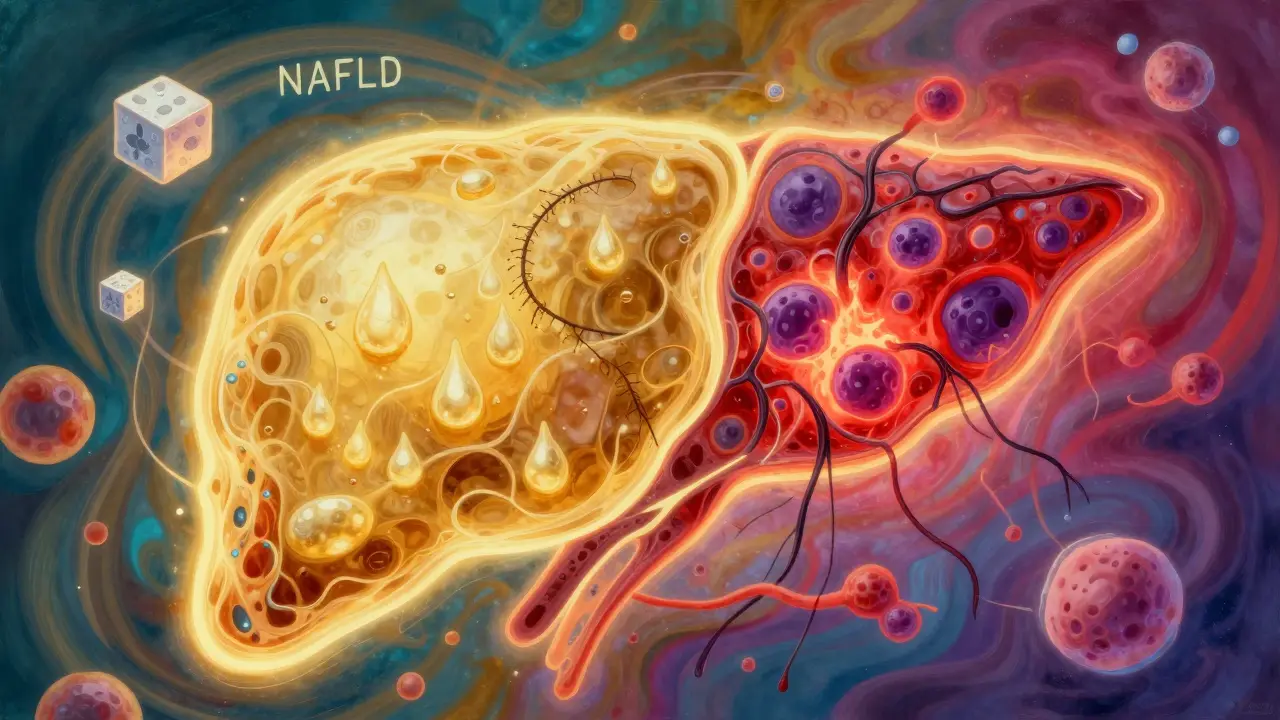
NAFLD - or Non-Alcoholic Fatty Liver Disease - is an umbrella term. It covers everything from simple fat accumulation to full-blown inflammation and scarring. Think of it like a spectrum. At one end is NAFL: just fat in the liver, with no damage. At the other end is NASH: fat plus inflammation, plus ballooned liver cells, plus the start of fibrosis. In 2023, experts updated the names to MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) and MASH (Metabolic Dysfunction-Associated Steatohepatitis), because the real problem isn’t alcohol - it’s metabolism. Insulin resistance, belly fat, high blood sugar, and high triglycerides are the culprits.
Here’s the key: NAFL doesn’t usually hurt your liver. A 2019 study following over 1,200 people for 15 years found only 12% of those with simple fatty liver developed serious scarring. But NASH? That’s different. In the same group, 42% of NASH patients progressed to advanced fibrosis. That’s more than three times the risk.
Fibrosis: The Silent Scarring Process
Fibrosis is the real threat. It’s not the fat itself that kills - it’s the scar tissue that replaces healthy liver cells. The liver can handle a lot, but once it starts turning into scar, it loses its ability to repair, filter toxins, and make proteins. Fibrosis is staged from 0 to 4:
- Stage 0: No scarring
- Stage 1: Tiny scars around veins
- Stage 2: Scarring spreading inward
- Stage 3: Bridging scars - connecting areas of damage
- Stage 4: Cirrhosis - the liver is mostly scar tissue
Stage 3 and 4 are the danger zones. People with stage 3 fibrosis have a 10-year liver-related death rate of 12-25%. Those with stage 0-2? Less than 2%. That’s the difference between managing a condition and facing life-threatening complications.
And here’s the scary part: NASH patients are 12 times more likely to die from liver problems than those with simple fatty liver. But even more surprisingly, the biggest cause of death in both groups isn’t liver disease - it’s heart disease. Over 40% of people with fatty liver die from cardiovascular issues. That’s why treating fatty liver isn’t just about the liver - it’s about fixing your whole metabolic health.
How Do You Know If You Have NASH?
There’s no simple blood test that says “NASH.” ALT and AST levels can be normal even when damage is happening. That’s why so many people are diagnosed late - their liver enzymes looked “fine” for years.
Doctors use a mix of tools:
- Ultrasound: Finds fat when it’s over 20-30% of the liver. Cheap, but misses mild cases.
- MRI-PDFF: Measures fat percentage accurately. Used in research and advanced clinics.
- FibroScan: A quick, painless scan that measures liver stiffness. A reading above 7.1 kPa suggests fibrosis.
- FIB-4 Score: Uses your age, platelet count, ALT, and AST. Over 1.3 means possible fibrosis. Over 2.67? High risk of advanced scarring.
- Liver biopsy: The only way to confirm NASH. It shows inflammation and ballooning - the hallmarks. But it’s invasive, carries small risks, and isn’t needed for everyone.
Most people don’t need a biopsy. If your FibroScan and FIB-4 are low, and you’re otherwise healthy, your doctor might just recommend lifestyle changes. But if you’re diabetic, obese, have high blood pressure, or your scores are high - biopsy might be the next step.
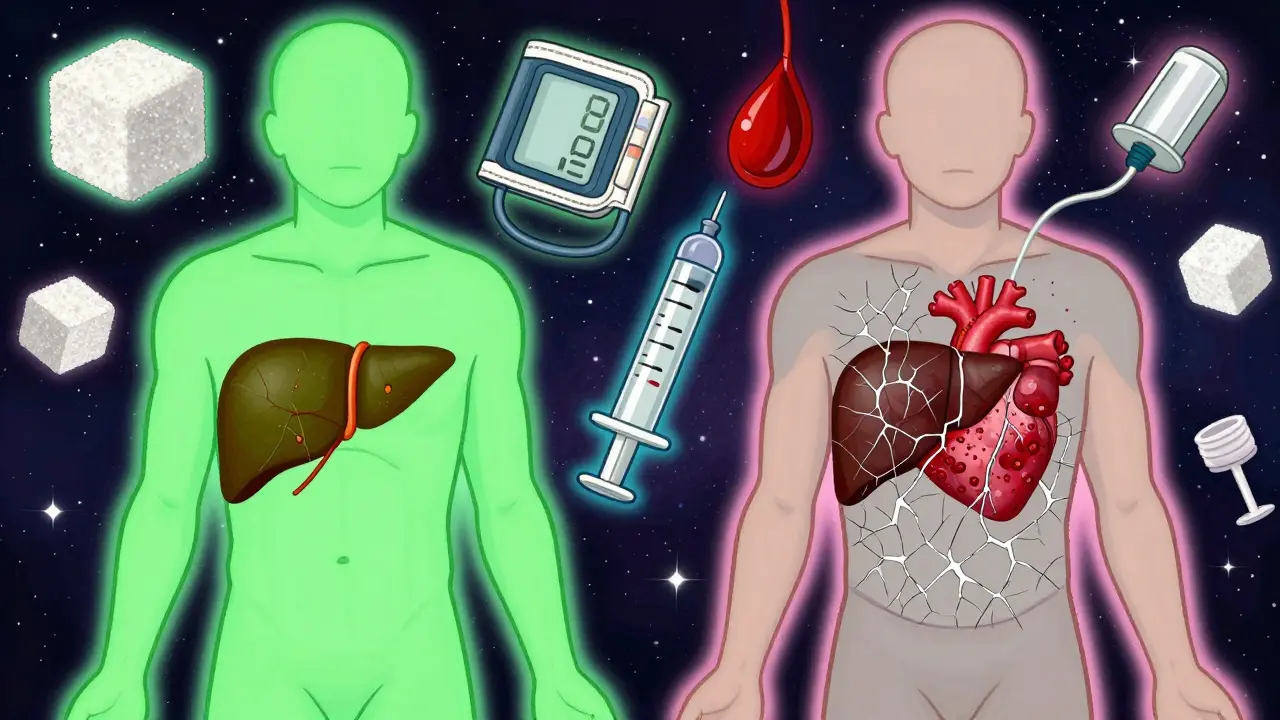
Who’s at Risk?
You don’t have to be overweight to have NASH, but it’s common. About 70-90% of NASH patients have a BMI over 30. Half to 70% have type 2 diabetes. Six in ten have high blood pressure. One in three has sleep apnea. These aren’t coincidences - they’re all part of the same metabolic mess.
Metabolic syndrome is the red flag. If you have three or more of these:
- Waist over 40 inches (men) or 35 inches (women)
- Triglycerides above 150 mg/dL
- HDL below 40 (men) or 50 (women)
- Blood pressure above 130/85
- Fasting blood sugar above 100 mg/dL
…then you’re at high risk. Screening isn’t optional - it’s essential. The American Association of Family Physicians recommends checking liver enzymes in anyone with metabolic syndrome, even if they feel fine.
What Can You Actually Do?
There’s no magic pill - yet. But there is a proven path.
Weight loss is the most powerful treatment. Losing just 5% of your body weight can reduce liver fat. Lose 7-10%, and you can reverse NASH entirely. One patient in the UK lost 14% of his weight over 18 months. His biopsy showed NASH had turned back to simple fatty liver. No medication. Just diet and movement.
Exercise matters, even without weight loss. A 2023 study showed 150 minutes of brisk walking a week reduced liver fat by 18% in NASH patients. Strength training helps too - muscle improves insulin sensitivity.
Diet? Cut the sugar. Cut the refined carbs. Cut the processed foods. Focus on whole foods: vegetables, lean protein, nuts, olive oil. Mediterranean diet patterns work best. Avoid alcohol completely - even small amounts worsen liver damage.
And yes - diabetes and blood pressure meds matter. Controlling your blood sugar and keeping your BP in check doesn’t just protect your heart. It protects your liver.
What’s New in Treatment?
For decades, the only treatment was lifestyle change. That’s still the foundation. But in March 2023, the FDA approved the first drug specifically for NASH: resmetirom (Rezdiffra). It’s for adults with moderate to advanced fibrosis (stage 2-3). In trials, 26% of patients had fibrosis improvement without worsening of NASH - compared to 10% on placebo.
Three other drugs are in late-stage trials. This is the first time in history that real, targeted treatment is on the horizon. But these aren’t cures. They’re tools - for people already at high risk. They don’t replace weight loss. They support it.
And the terminology change? MASLD and MASH aren’t just new names. They’re a shift in thinking. It’s not “non-alcoholic” - it’s metabolic. That means doctors now look at your whole body, not just your liver. Your fat distribution, your insulin levels, your heart health - they’re all part of the picture.
Why This Matters Right Now
By 2030, over a third of the world’s population could have MASLD. In the U.S., liver transplants due to NASH are expected to double. The economic cost? Over $100 billion a year - mostly from advanced disease.
But here’s the hopeful part: if you catch it early - before fibrosis - you can turn it around. Studies show 90% of people who lose 7-10% of their weight reverse NASH. Eighty-five percent improve their fibrosis. That’s not a guess. That’s data.
The problem isn’t lack of knowledge. It’s lack of action. Too many people wait until their liver is failing. Too many doctors don’t screen because they think “it’s just fatty liver.” But fatty liver isn’t harmless. It’s a warning sign - loud and clear - that your metabolism is out of balance.
If you’re overweight, diabetic, or have high blood pressure - get tested. Ask for an ALT check. Ask about FibroScan. Don’t wait for symptoms. By the time you feel tired or bloated, the damage may already be there.
Your liver doesn’t scream. It whispers. Listen before it’s too late.
Is NAFLD the same as NASH?
No. NAFLD is the broad term for fat in the liver without alcohol use. NASH is a more serious form that includes inflammation and liver cell damage. Think of NAFLD as the umbrella - NASH is one type under it. NASH carries a much higher risk of scarring and liver failure.
Can you have NASH without being overweight?
Yes. While most NASH patients are overweight or obese, about 10-20% have normal weight. This is called “lean NASH.” It’s linked to insulin resistance, genetics, or gut health issues. Don’t assume you’re safe just because you’re thin.
How do I know if I have fibrosis?
Blood tests alone can’t confirm it. FibroScan is the most common non-invasive test - it measures liver stiffness. FIB-4 score, using your age, platelets, ALT, and AST, is another tool. If either is high, your doctor may recommend a biopsy for a definitive diagnosis. Early fibrosis has no symptoms.
Is there a cure for NASH?
There’s no approved cure yet, but NASH can be reversed - especially in early stages. Losing 7-10% of your body weight, eating a whole-food diet, and exercising regularly can eliminate inflammation and even reduce scarring. The new drug resmetirom helps in moderate to advanced cases, but lifestyle change remains the most effective tool.
Should I get a liver biopsy?
Not everyone needs one. Biopsies are usually reserved for people with high risk - like those with diabetes, high FibroScan or FIB-4 scores, or signs of advanced disease. It’s invasive and carries small risks, so doctors use it only when the results will change your treatment plan.
Can I reverse liver damage from NASH?
Yes - if caught early. Studies show that losing 7-10% of body weight can reverse NASH in 90% of cases and improve fibrosis in 85%. Even small changes matter. The liver is one of the few organs that can regenerate. The sooner you act, the better your chances.


Eli Kiseop
February 1, 2026 AT 19:15So basically if you got belly fat and eat pizza like its a sport your liver is just silently screaming for help
no pain no gain right until its too late