Millions of people take statins to lower cholesterol and reduce heart disease risk. At the same time, nearly half of all Americans take vitamin D supplements - often for bone health, immune support, or because they’ve heard it might help with statin side effects. But does vitamin D actually help with statin-related muscle pain? And can statins mess with your vitamin D levels? The answer isn’t simple. Research gives conflicting signals, and what patients report often doesn’t match what clinical trials show.
How Statins and Vitamin D Are Connected
Statins work by blocking an enzyme called HMG-CoA reductase, which your body uses to make cholesterol. Vitamin D, specifically vitamin D3 (cholecalciferol), is made from cholesterol in your skin when sunlight hits it. So, logically, if statins lower cholesterol, they might also lower vitamin D. But that’s not what most studies find.
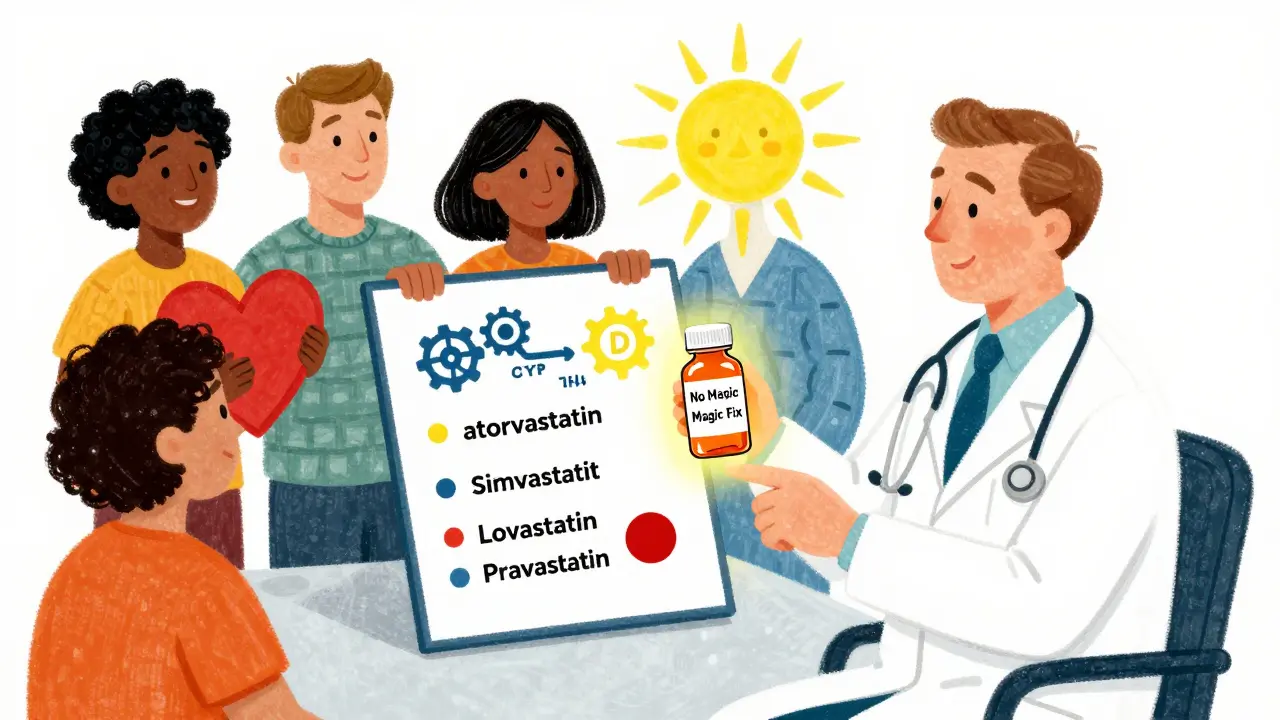
Instead, the real interaction is more complex. Some statins - like atorvastatin, simvastatin, and lovastatin - are broken down by the same liver enzyme (CYP3A4) that processes vitamin D. This raises the question: do they compete? Could one block the other? A 2012 study found that rosuvastatin and atorvastatin actually raised vitamin D levels in patients over just eight weeks. Researchers thought maybe these statins were boosting how much vitamin D your body absorbs. Other statins, like pravastatin and fluvastatin, don’t use that enzyme much - and they didn’t change vitamin D levels at all.
Does Vitamin D Help with Statin Muscle Pain?
This is the biggest question for patients. Around 10-20% of people on statins report muscle aches, weakness, or cramps. Many try vitamin D because it’s safe, cheap, and widely available. But the largest, most rigorous study to date - the VITAL trial substudy in 2022 - found no difference.
The study followed 2,083 people who started statins. Half took 2,000 IU of vitamin D daily. The other half took a placebo. After a year, muscle symptoms appeared in 31% of both groups. Even among people with low vitamin D levels (under 20 ng/mL), the rates were nearly identical: 33% in the vitamin D group, 35% in the placebo group. The study didn’t find any benefit, no matter how low someone’s vitamin D started.
That’s a hard result to ignore. The American College of Cardiology now says routine vitamin D supplementation for statin users isn’t recommended. The European Society of Cardiology agrees: while deficiency might make muscle pain worse, giving more vitamin D doesn’t fix it.
But Why Do So Many People Say It Works?
Despite the science, patient stories are loud. On Reddit’s r/Statins forum, over half of the 1,247 people surveyed said vitamin D helped their muscle pain. On Drugs.com, 37% of 1,852 users believed it made a difference. Mayo Clinic surveys show that 61% of people who quit statins because of muscle pain thought vitamin D would’ve helped.
Why the gap? One reason is the placebo effect. When you try something new, your brain expects relief - and sometimes, that’s enough. Another is timing. Some people start vitamin D right after symptoms begin, then feel better weeks later. They credit the supplement, but maybe their body just adjusted to the statin over time.
Also, a small group of patients - those with severe deficiency (under 12 ng/mL) - might genuinely improve. A few case reports from the American Heart Association describe muscle pain disappearing after high-dose vitamin D. But these are rare. The VITAL trial specifically looked at people with low levels and still found no benefit.

Do Statins Lower Vitamin D Levels?
Again, the data is mixed. Some studies say yes. A 2018 study of 125 people found statin users had much lower vitamin D levels (15.8 ng/mL) than non-users (20.6 ng/mL). They also had more deficiency: 72% of statin users were deficient, compared to 49% of controls.
But other studies say the opposite. A 2019 study found statin users had higher vitamin D levels than non-users. Atorvastatin users had the highest levels (23 ng/mL on average). Why the contradiction? It might depend on the statin type, diet, sun exposure, or even genetics.
One theory: statins might increase the activity of proteins that move cholesterol (and vitamin D) into your bloodstream. Another: people on statins might be more health-conscious - they eat better, get more sun, take supplements. That could explain higher levels.
Bottom line: statins don’t reliably lower vitamin D. In fact, some types might slightly raise them. But this doesn’t mean you’re getting enough. Many people - statin users or not - are still deficient.
Which Statins Interact With Vitamin D?
Not all statins are the same. If you’re on atorvastatin, simvastatin, or lovastatin, you’re using a statin metabolized by CYP3A4. This is the enzyme that also processes vitamin D. Some researchers think this might lead to a two-way interaction: vitamin D supplements could affect how your body breaks down the statin, and the statin could affect how your body uses vitamin D.
A 2015 study found that people taking 800 IU of vitamin D daily had lower levels of atorvastatin in their blood. That might mean the statin is less effective. But the study was small. No one has proven this changes heart attack risk.
On the other hand, rosuvastatin and pravastatin are processed differently. They don’t use CYP3A4 much. So if you’re on one of those, vitamin D is unlikely to interfere. That’s why some doctors suggest switching statins if muscle pain persists - not because of vitamin D, but because different statins have different side effect profiles.
What Should You Do?
Here’s what the evidence says, plain and simple:
- If you have muscle pain on a statin, don’t assume vitamin D will fix it. The best evidence says it won’t.
- If your vitamin D level is below 20 ng/mL, supplementing for bone and immune health is still a good idea - but not because it helps your muscles.
- If you’re on atorvastatin, simvastatin, or lovastatin, talk to your doctor before taking more than 1,000 IU of vitamin D daily. There’s a small chance it could affect how the drug works.
- Don’t stop your statin because you think vitamin D will help. Statins prevent heart attacks and strokes. The benefit far outweighs the risk of muscle pain for most people.
- If muscle pain is bad, ask about switching statins or lowering the dose. Those are proven strategies.
The American Pharmacists Association says: monitor vitamin D levels in people with persistent muscle symptoms. But don’t give supplements just to treat those symptoms. The science doesn’t support it.
What’s Next?
Research is still evolving. The PRECISION trial, which started in 2023 and will finish in late 2025, is testing whether vitamin D helps only people with very low levels (under 12 ng/mL). Early data might show a small group benefits - but it won’t change the big picture.
Another angle: genetics. A 2023 study from Johns Hopkins found that people with certain gene variations in the CYP2R1 enzyme (which turns vitamin D into its active form) respond differently to statins. This could explain why some people have muscle pain and others don’t - and why vitamin D helps some and not others.
For now, the advice is clear: take vitamin D if you’re deficient. But don’t expect it to fix statin muscle pain. And don’t stop your statin because of it.
Can vitamin D supplements prevent statin muscle pain?
No, current evidence shows vitamin D supplements do not prevent or reduce statin-associated muscle symptoms. The largest randomized trial (VITAL substudy, 2022) found no difference in muscle pain between people taking 2,000 IU of vitamin D daily and those taking a placebo, even among those with low baseline vitamin D levels.
Do statins lower vitamin D levels in the body?
The effect varies by statin type and individual factors. Some studies show statin users have lower vitamin D levels, while others show higher levels - especially with atorvastatin and rosuvastatin. There’s no consistent pattern. Statins don’t reliably lower vitamin D, and some may even increase it slightly due to effects on cholesterol transporters.
Which statins interact with vitamin D supplements?
Atorvastatin, simvastatin, and lovastatin are metabolized by the CYP3A4 enzyme, which also processes vitamin D. This creates a potential for interaction. Rosuvastatin, pravastatin, and fluvastatin use different pathways and are less likely to interact. If you’re on one of the CYP3A4-metabolized statins and taking high-dose vitamin D, talk to your doctor about possible effects on drug levels.
Should I take vitamin D if I’m on a statin?
Only if your blood test shows you’re deficient (under 20 ng/mL). Vitamin D is important for bone health, immunity, and overall well-being. But taking it to relieve statin muscle pain won’t work. Don’t take high doses without a reason - and don’t stop your statin because you think vitamin D will help.
Why do doctors still recommend vitamin D for statin users?
Many doctors recommend it because patients ask for it - and because they believe it might help. A 2023 Medscape survey found 47% of primary care physicians still suggest vitamin D for statin users due to patient demand, even though clinical guidelines don’t support it. It’s a gap between patient expectations and scientific evidence.