Vitamin D & Statin Tolerance Calculator
Enter your vitamin D level to see your deficiency status and evidence-based recommendations.
Millions of people take statins to lower their cholesterol and prevent heart attacks. But for up to 29% of them, the medication causes muscle pain, weakness, or cramps-enough to make them quit. For years, doctors noticed something odd: many of these patients also had low vitamin D. Some even saw symptoms disappear after giving them vitamin D supplements. It sounded too good to be true. And now, after years of conflicting studies, we finally have the clearest answer yet.
Why This Matters More Than You Think
Statin therapy cuts heart attack risk by 25-35% in high-risk patients. That’s huge. But if someone stops taking their statin because of muscle pain, that protection vanishes. And here’s the problem: muscle pain from statins is often vague. It’s not always clear if it’s the drug, low vitamin D, aging, or just coincidence. Many patients blame the statin and quit-even when the real issue might be something simple like low vitamin D. In clinical practice, it’s common to check vitamin D levels in people who report muscle pain on statins. Why? Because back in 2009, a small study found that 92% of patients with low vitamin D and statin-related muscle pain felt better after taking supplements. That got everyone’s attention. Since then, dozens of doctors started testing and treating-sometimes with dramatic results.The Promise: Vitamin D Fixes Statin Muscle Pain
A 2017 study looked at 120 patients who had previously stopped statins because of muscle symptoms. Nearly all of them had vitamin D levels below 20 ng/mL-what’s considered deficient. After giving them 1,000-2,000 IU of vitamin D daily for 4-8 weeks, their levels rose above 30 ng/mL. Then, they tried statins again. The results? 90% of those with baseline deficiency could tolerate statins after supplementation. That’s not a small number. For patients who’d tried three or more statins and failed, this was life-changing. Pravastatin and rosuvastatin worked best after vitamin D correction. The researchers concluded that low vitamin D might be a hidden cause of statin intolerance. Other smaller studies backed this up. One in 2015 found that 53% of statin-intolerant patients could restart statins after vitamin D repletion. In clinics, doctors reported patients who’d been off statins for years suddenly able to take them again-no pain, no problem. The theory? Vitamin D helps muscles function better. Low levels can cause weakness and pain on their own. Add a statin, and the muscle stress becomes too much.The Problem: A Big Trial Says No
Then came the 2022 JAMA Cardiology study-and it changed everything. This wasn’t a small observation. It was a randomized, double-blind, placebo-controlled trial with over 2,000 participants. All were starting statins. Half got 2,000 IU of vitamin D daily. Half got a dummy pill. No one knew who got what. After a year, the results were clear: 31% of people in both groups developed muscle symptoms. 13% stopped their statin in both groups. No difference. Zero. Not even a hint. This is the gold standard of medical evidence. Unlike earlier studies that just looked at people who already had symptoms, this one followed people from the start. It didn’t matter if you were low in vitamin D or not-you were just as likely to have muscle pain. The authors didn’t hold back: “Vitamin D supplementation did not prevent statin-associated muscle symptoms.” That’s a hard blow to the idea that fixing vitamin D will fix statin tolerance.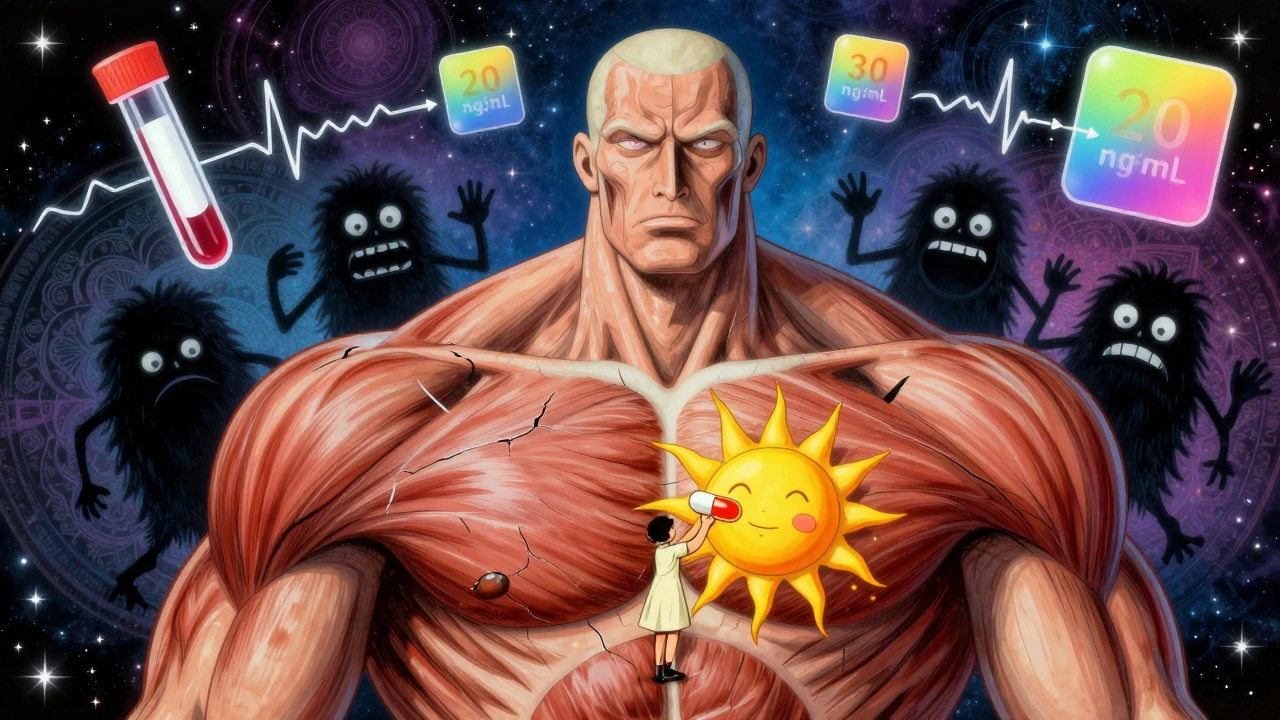
Why Do the Studies Conflict?
The answer lies in how the studies were done. The positive ones were mostly observational. They looked at people who already stopped statins because of pain. Then they checked vitamin D levels. When those levels went up, pain went down. But here’s the catch: when you feel better after taking a supplement, you might think it’s because of the supplement. But what if your pain was already fading? Or what if you were more active, sleeping better, or just more hopeful after getting a “treatment”? That’s the placebo effect-and it’s powerful. The JAMA study avoided that trap. It didn’t wait for people to quit. It gave vitamin D from day one. And it didn’t let people know if they were getting it. That’s the only way to know if it truly works. Also, vitamin D levels in the JAMA study were mostly normal at the start. Most participants weren’t deficient. So maybe vitamin D only helps people who are truly low-like those in the 2017 study, who were all under 20 ng/mL. The JAMA trial didn’t focus on that group. Maybe that’s the missing piece.What Should You Do If You’re on Statins and Have Muscle Pain?
Here’s the practical bottom line:- If you’re on a statin and have unexplained muscle pain, ask your doctor to check your vitamin D level. It’s a simple blood test.
- If your level is below 20 ng/mL, correcting it is a low-risk, low-cost move. Even if it doesn’t fix your statin tolerance, it helps your bones, immune system, and overall muscle health.
- If your level is above 30 ng/mL, taking extra vitamin D probably won’t help your muscle pain.
- Don’t assume vitamin D is the fix. Other causes-like thyroid problems, kidney issues, or even just overexertion-can mimic statin side effects.
Which Statins Are Easier to Tolerate?
Some statins are more likely to cause muscle pain than others. That’s true even without vitamin D issues.- Pravastatin and rosuvastatin are least likely to cause muscle problems. They’re not heavily processed by liver enzymes that can build up toxins.
- Atorvastatin is common and effective, but it’s metabolized differently-and some studies link it to slightly higher muscle symptom rates.
- Simvastatin and lovastatin are older and more likely to cause issues, especially at higher doses.

Is Vitamin D Supplementation Safe?
Yes. Taking 1,000-2,000 IU of vitamin D3 daily is safe for most people. The body naturally makes vitamin D from sunlight, and supplements just help fill the gap-especially in places like the UK, where sunlight is limited for half the year. But more isn’t better. Taking over 4,000 IU daily long-term can raise calcium levels and harm your kidneys. Stick to the standard dose unless your doctor says otherwise.What’s Next?
The science isn’t settled. The JAMA study was big and well-run, but it didn’t test people with severe vitamin D deficiency. That’s a gap. Some researchers believe the real benefit might be hidden in that group. Future studies need to focus on patients with vitamin D levels below 20 ng/mL who are starting statins. Only then can we know if supplementation helps those who need it most. Until then, the safest approach is this: test vitamin D if you have muscle pain. If it’s low, fix it. If your pain goes away, great. If it doesn’t, don’t blame vitamin D. Try a different statin. Talk to your doctor about dose adjustments. Don’t quit without exploring options.Why This Debate Matters Beyond the Lab
This isn’t just about one nutrient and one drug. It’s about how medicine works. We want simple fixes. Low vitamin D? Take a pill. Problem solved. But biology doesn’t work that way. Muscle pain on statins is complex. It’s influenced by genetics, age, activity level, other medications, and even how we think about our bodies. The fact that millions of people are on statins means even a small percentage of intolerance affects public health. If we can help even 10% of those people stay on their medication, we prevent thousands of heart attacks. That’s why this debate continues. Even if vitamin D doesn’t help everyone, it might help someone. And in medicine, that’s worth looking for.Can low vitamin D cause muscle pain even without statins?
Yes. Vitamin D deficiency is directly linked to muscle weakness, fatigue, and pain in people who aren’t taking statins. Studies show that correcting low vitamin D levels improves muscle strength and reduces discomfort in many cases. This is why doctors check vitamin D in anyone with unexplained muscle symptoms-not just statin users.
Should everyone on statins take vitamin D supplements?
No. Only take vitamin D if your blood test shows a deficiency (below 20 ng/mL). For people with normal levels, extra vitamin D won’t prevent statin muscle pain. Taking supplements without a need offers no benefit and could lead to unnecessary costs or risks over time.
What’s the best dose of vitamin D for someone on statins?
For deficiency, most doctors recommend 1,000-2,000 IU of vitamin D3 daily for 8-12 weeks to raise levels into the normal range (30-50 ng/mL). After that, a maintenance dose of 600-1,000 IU daily is usually enough. Always confirm your levels with a blood test before and after treatment.
If vitamin D doesn’t help, what else can I try for statin muscle pain?
Switch to a different statin-pravastatin or rosuvastatin are often better tolerated. Lower the dose or take it every other day. Some people benefit from coenzyme Q10 supplements, though evidence is mixed. Talk to your doctor about checking for other causes like thyroid dysfunction or electrolyte imbalances. Never stop statins without medical advice.
Can statins actually raise vitamin D levels?
Some studies suggest this might be possible. One 2019 study found that people taking statins had slightly higher vitamin D levels than those not on them. The reason isn’t clear-maybe statins affect how the body processes vitamin D, or perhaps people on statins are more health-conscious overall. This could mean that low vitamin D isn’t the cause of muscle pain, but a side effect of stopping statins. More research is needed.





Sean McCarthy
December 1, 2025 AT 05:44My doctor checked my vitamin D last year when I had statin muscle pain. It was low. I took the supplement for two months. Pain went away. I don't care what big studies say. This worked for me.
Matt Dean
December 2, 2025 AT 05:44Of course the JAMA study says no. Big pharma funded it. The 2017 study had real patients. This one had people with normal vitamin D. Of course it failed. They didn't test the right group. Classic.
Walker Alvey
December 3, 2025 AT 20:05So we're supposed to believe that taking a $0.05 pill fixes a multi-billion dollar drug's side effects? The placebo effect is stronger than your vitamin D levels. Also your bones are fine. Stop taking supplements.
Dennis Jesuyon Balogun
December 5, 2025 AT 03:55The reductionist paradigm fails here. Vitamin D deficiency is a biomarker of systemic dysregulation-not a causal agent per se. Statin-induced myopathy is multifactorial: mitochondrial dysfunction, CoQ10 depletion, genetic polymorphisms in SLCO1B1, and epigenetic modulation of muscle protein expression. To isolate vitamin D as a panacea is reductionist scientism. The JAMA trial's null result is epistemologically robust precisely because it controlled for confounding variables that observational studies ignorantly conflated with causation.
Grant Hurley
December 5, 2025 AT 17:04i took pravastatin after my doc gave me vit d and it was a game changer. no more leg cramps at night. also i started walking more. maybe it was the walking? who knows. but i feel better. thats what matters. 🙌
Souvik Datta
December 7, 2025 AT 12:09In my clinical experience, the key is not just vitamin D levels but the patient's baseline activity and metabolic health. Many patients with low vitamin D are sedentary, overweight, or have subclinical hypothyroidism. When we correct vitamin D without addressing these, results are mixed. But when we combine supplementation with lifestyle intervention-movement, sleep, nutrition-the response is dramatic. The JAMA study missed this holistic context.
Priyam Tomar
December 9, 2025 AT 02:30Everyone’s acting like vitamin D is magic. You know what fixes statin pain? Stopping statins. The real problem is doctors pushing drugs instead of asking why someone has high cholesterol in the first place. Diet? Genetics? Stress? Nah. Let’s just pop a pill and call it a day.
Jack Arscott
December 9, 2025 AT 16:14My mom took vit D and switched to rosuvastatin after years of pain. She’s been on it for 3 years now. No issues. I’m not saying it works for everyone, but for some? It’s a miracle. 🙏
Adrian Barnes
December 11, 2025 AT 01:14It is not merely statistically insignificant; it is epistemologically definitive. The JAMA trial, with its rigorous methodology, nullifies the entire corpus of observational literature predicated upon selection bias, confirmation bias, and regression to the mean. To continue promoting vitamin D supplementation as a therapeutic intervention for statin intolerance constitutes medical malpractice by omission of evidence-based standards.
Lucinda Bresnehan
December 12, 2025 AT 01:35i had the muscle pain and thought it was the statin, so i quit. then i got really tired and my knees hurt. doctor said my vit d was 12. after 3 months of supplements, i felt like a new person. i restarted the statin and no pain. i dont know why it worked but it did. thanks for writing this, i needed to hear it.
Shannon Gabrielle
December 14, 2025 AT 00:01Of course the study says no. They didn’t test people who actually live in the dark like the rest of us. I live in Seattle. My vitamin D is lower than my bank account. If you think sunshine and a $2 pill won’t help when you’re dragging your legs around like a zombie, you’re the problem.
ANN JACOBS
December 14, 2025 AT 22:39The most profound insight here is not about vitamin D or statins-it’s about the tension between the individual experience and the collective evidence. One person’s life-changing relief is another person’s placebo. Medicine must honor both. We cannot dismiss the grandmother who walks again after years of pain because a randomized trial didn’t show population-wide benefit. Nor can we prescribe supplements to millions who don’t need them because one person felt better. The truth lies in the nuanced middle: test, treat the deficient, respect the data, and never stop listening to the patient. That’s not just good medicine. That’s human medicine.