Proton pump inhibitors, or PPIs, are among the most common medications prescribed for heartburn, acid reflux, and ulcers. Brands like Prilosec, Nexium, and Protonix have become household names. For many people, they work quickly and effectively-so well, in fact, that patients often keep taking them for months or even years without ever checking if they still need them. But what happens when you take PPIs for too long? And how do you know when it’s time to stop?
How PPIs Work and Why They’re So Popular
PPIs block the final step of stomach acid production. They target the proton pumps in the stomach lining-tiny engines that pump acid into your stomach to help digest food. By shutting these down, PPIs reduce acid by up to 90%. That’s why they’re more effective than older drugs like ranitidine or famotidine, which only block part of the acid system.
They’re prescribed for conditions like GERD, peptic ulcers, and to protect the stomach from NSAIDs like ibuprofen or aspirin. For people with severe esophagitis, PPIs can be life-changing. But for others-like those with occasional heartburn or mild indigestion-they’re often overused. Studies show that up to 70% of people taking PPIs don’t actually have a diagnosis that justifies long-term use.
The Hidden Risks of Long-Term Use
While PPIs are safe for short-term use-typically 4 to 8 weeks-taking them for more than a year raises real concerns. The FDA has issued seven safety warnings since 2010, and many of these risks are underreported or misunderstood.
Fracture risk is one of the most well-documented dangers. Long-term PPI users have a 40% to 55% higher chance of hip fractures, especially if they’re over 65 or have osteoporosis. The reason? PPIs interfere with calcium absorption. The good news? This risk drops back to normal within two years of stopping the medication.
Magnesium deficiency is rarer but more serious. It affects about 1 in 100 long-term users. Symptoms include muscle cramps, irregular heartbeat, fatigue, and seizures. The FDA now recommends checking magnesium levels if you’ve been on PPIs for over a year. If levels drop too low, you may need supplements or to stop the drug entirely.
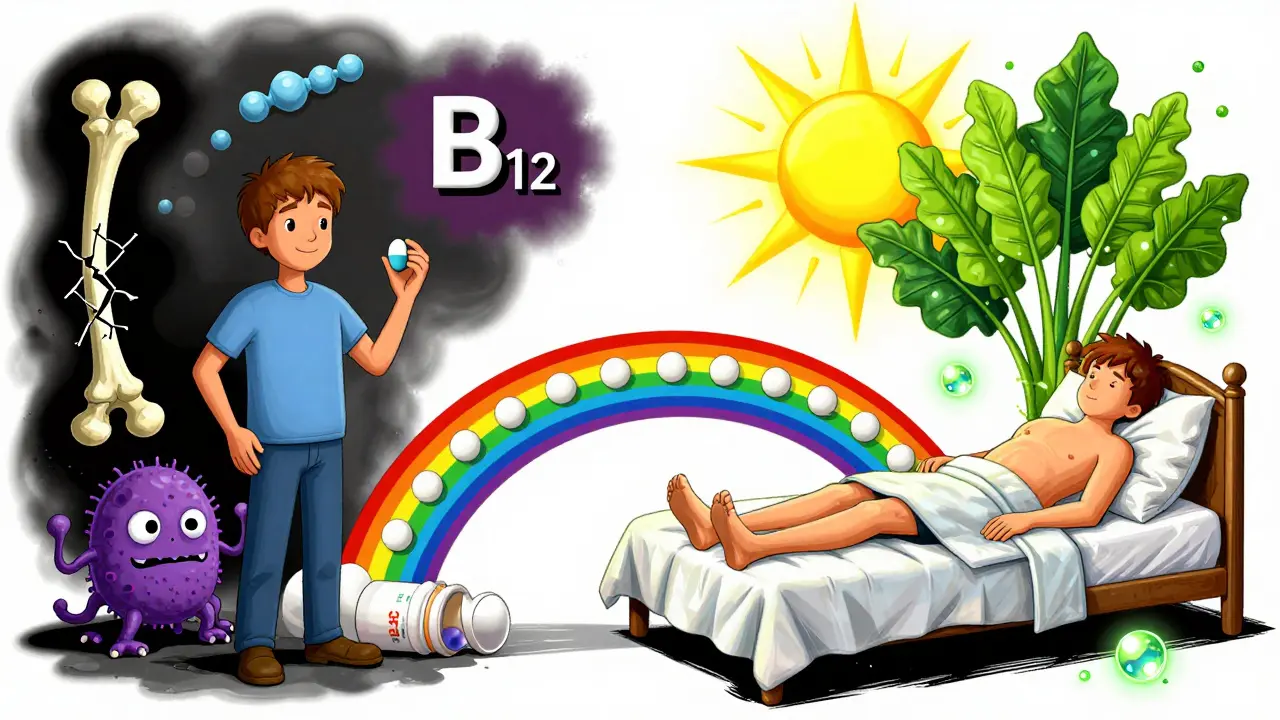
Vitamin B12 deficiency is another silent issue. About 1 in 7 long-term users develop this. B12 is critical for nerve function and blood cell production. Without it, you can feel numb, dizzy, or mentally foggy. PPIs reduce stomach acid, which is needed to pull B12 out of food. Blood tests can catch this early, and supplements usually fix it.
C. difficile infection is a serious gut infection that can cause severe diarrhea and colitis. PPIs raise your risk by 1.7 to 2 times, especially if you’re hospitalized or on antibiotics. The lower stomach acid lets harmful bacteria survive and multiply.
Some studies have linked PPIs to kidney disease, dementia, and heart problems. But the evidence here is mixed. Many of these studies didn’t control for other health issues-like diabetes, high blood pressure, or smoking-that could be the real cause. Experts like Dr. William Ravich from Yale say, “Most of these links are associations, not causes.” That doesn’t mean you should ignore them, but it does mean you shouldn’t panic.
Rebound Acid: The Hidden Trap When Stopping
One of the biggest reasons people can’t stop PPIs isn’t because they still need them-it’s because stopping makes their symptoms worse. This is called rebound acid hypersecretion. After months or years of suppressing acid, your stomach overcompensates. It produces even more acid than before, leading to intense heartburn, nausea, and bloating.
Up to 80% of people who quit PPIs cold turkey experience this. It usually lasts 2 to 8 weeks. Many patients think the PPI was working, so they go right back on it. But the truth? The acid wasn’t coming back because their condition returned-it was because their body was reacting to the sudden absence of the drug.
When and How to Stop PPIs Safely
You should consider stopping PPIs if:
- You’ve been taking them for more than 8 weeks without a confirmed diagnosis
- You’re using over-the-counter PPIs for longer than 14 days, more than once every 3 months
- You have no symptoms but are taking it “just in case”
- You’re on multiple medications and want to reduce pill burden
Stopping isn’t as simple as skipping a dose. Here’s how to do it right:
- Work with your doctor. Don’t quit on your own.
- Reduce your dose by half every 1-2 weeks. For example, go from 20mg daily to 10mg daily, then 10mg every other day.
- Switch to on-demand use. Take the PPI only when you have symptoms, not daily.
- Try H2 blockers like famotidine (Pepcid) or ranitidine (if available) during the transition. They’re less potent but help ease the rebound.
- Use antacids like Tums or Gaviscon for breakthrough symptoms. They’re safe for occasional use.
- Give it 4-8 weeks. Rebound symptoms fade over time. Most people are symptom-free by week 6.
Some patients need a “drug holiday”-a 2- to 4-week break every 6-12 months-to see if they still need the medication. If symptoms stay gone, you may not need to restart.
Alternatives to PPIs
You don’t need to live with acid reflux-but you also don’t need to rely on PPIs forever.
Lifestyle changes are the first line of defense:
- Don’t eat 3 hours before bed
- Avoid spicy, fatty, or acidic foods
- Loosen tight clothing around your waist
- Elevate the head of your bed by 6 inches
- Quit smoking and limit alcohol
- Lose weight if you’re overweight-just 10 pounds can make a big difference
H2 blockers like famotidine or nizatidine are weaker than PPIs but safer for long-term use. They’re great for occasional heartburn or as a bridge during tapering.
Prokinetic agents like metoclopramide help your stomach empty faster, reducing reflux. But they have side effects and aren’t for everyone.
Newer drugs like vonoprazan (a potassium-competitive acid blocker) are being studied. They work faster than PPIs and may have fewer long-term risks. But they’re not yet widely available in the U.S. and their safety over 10+ years is unknown.
Who Should Stay on PPIs?
Not everyone should stop. If you have:
- Severe erosive esophagitis
- A history of bleeding ulcers
- Barrett’s esophagus
- Chronic use of NSAIDs like ibuprofen or naproxen
Then long-term PPIs may still be necessary. But even then, you should be on the lowest effective dose and have your condition reviewed at least once a year.
What to Do If You’re Already on PPIs Long-Term
If you’ve been taking PPIs for more than a year, here’s your action plan:
- Ask your doctor: “Do I still need this?”
- Request a magnesium and B12 blood test
- Review your symptoms-are they truly acid-related, or could they be something else?
- Start tracking your heartburn triggers with a food and symptom journal
- Try a 2-week taper plan under supervision
Many people are surprised to find they’ve been taking PPIs for years without ever having a follow-up. That’s not normal. Medications aren’t meant to be taken forever unless absolutely necessary.
Final Thoughts
PPIs are powerful tools-but they’re not harmless. They’re not candy. They’re not “just for heartburn.” For some, they’re life-saving. For many more, they’re a crutch that masks the real issue: diet, weight, or lifestyle.
Stopping PPIs isn’t about fear. It’s about responsibility. You owe it to your body to question every long-term medication. If you’ve been taking one for more than a year, it’s time to talk to your doctor-not because you’re in danger, but because you deserve to be sure you still need it.
Most people who taper off PPIs safely don’t go back. Their symptoms improve. Their body recalibrates. And they feel better without the pills.
Can I stop taking PPIs cold turkey?
No, stopping abruptly can cause severe rebound acid reflux, with symptoms worse than before. Up to 80% of long-term users experience this. Always taper down slowly under medical supervision-reduce the dose by half every 1-2 weeks, then switch to on-demand use before stopping completely.
How long does it take to get off PPIs safely?
It usually takes 4 to 8 weeks to fully stop PPIs without severe rebound. The first 2 weeks involve reducing the dose, the next 2-4 weeks involve switching to on-demand use, and the final 1-2 weeks are for complete discontinuation. Rebound symptoms typically fade by week 6.
Are over-the-counter PPIs safer than prescription ones?
No. OTC PPIs have the same active ingredients and risks as prescription versions. The FDA limits OTC use to 14 days every 3 months because long-term self-medication leads to dependency and hidden side effects. Just because they’re available without a prescription doesn’t mean they’re safe for daily, long-term use.
Can PPIs cause kidney damage?
PPIs can cause acute interstitial nephritis-a rare but serious kidney inflammation-especially within the first 3 months of use. Chronic kidney disease is more controversial. While some studies show a link, others find no increased risk after adjusting for age, diabetes, and high blood pressure. If you’re on PPIs long-term, get your kidney function checked yearly.
Do PPIs increase the risk of dementia?
Some early studies suggested a link, but newer, higher-quality research hasn’t confirmed it. Many of those studies didn’t account for other factors like age, diabetes, or poor diet. Experts agree there’s no strong evidence that PPIs cause dementia, but the possibility can’t be ruled out entirely. If you’re concerned, talk to your doctor about whether you still need the medication.
What are the best alternatives to PPIs for heartburn?
For occasional heartburn, antacids like Tums or H2 blockers like famotidine (Pepcid) work well. For long-term management, focus on lifestyle changes: avoid late meals, reduce fatty/spicy foods, lose weight if needed, elevate your bed, and quit smoking. These changes often eliminate the need for medication entirely.
How do I know if I really need PPIs?
If you’ve been taking PPIs for more than 8 weeks without a confirmed diagnosis-like an endoscopy showing esophagitis or a positive H. pylori test-you likely don’t need them. Most people with mild heartburn improve with diet, weight loss, and occasional H2 blockers. Ask your doctor: “What was my diagnosis?” and “Has it been confirmed?”





Jacob Milano
January 4, 2026 AT 11:48Wow, this is one of those posts that makes you rethink everything you thought you knew about heartburn meds. I’ve been on Nexium for three years ‘just in case’-turns out I just needed to stop eating pizza at midnight and sleep with my head on a brick. Who knew?
Rebound acid is real. I tried quitting cold turkey once and felt like my stomach was hosting a rave. Two weeks of half-doses and Pepcid saved me. Now I’m symptom-free and actually sleep through the night. My doctor was shocked I’d been on it so long without a follow-up.
Also, B12 deficiency? I had numb fingers and brain fog for months. Thought it was stress. Turns out my stomach was too quiet to pull the vitamin out of food. Blood test fixed it. PPIs aren’t candy. They’re like putting a blanket over a fire-you think it’s gone, but it’s just waiting to explode.
And yeah, the fracture risk? My grandma broke her hip after 5 years on Prilosec. No falls. No accidents. Just calcium being ignored by her body. Scary stuff.
But here’s the thing: if you’ve got Barrett’s or ulcers? Don’t stop. This isn’t anti-PPI propaganda-it’s anti-complacency. Use them like a tool, not a lifestyle.
Also, vonoprazan sounds like sci-fi. When’s it coming to the States? I’m ready to upgrade.
Cassie Tynan
January 6, 2026 AT 00:46So let me get this straight-we’re told to take a drug for ‘heartburn’ that’s basically a chemical lobotomy for your stomach… and then we’re surprised when your body starts acting like a confused toddler who just lost its pacifier?
Of course you get rebound. Of course your B12 drops. Of course your bones turn to dust. You didn’t fix the problem-you silenced the messenger.
It’s like giving someone a sedative because they’re screaming about a fire… then wondering why they’re still burning.
Also, ‘OTC PPIs are safer’? LOL. The FDA lets you buy them like gum because they don’t want to deal with the lawsuits when you end up on dialysis. They’re not protecting you-they’re profiting.
Wake up. Your body is not a vending machine. You don’t get to insert cash and expect it to fix your life choices.
Peyton Feuer
January 7, 2026 AT 17:14just tried to quit my ppi last year and thought i was gonna die from heartburn. turned out it was just rebound. took 6 weeks to feel normal again. now i use tums when i eat too much mexican food and it’s fine. also started sleeping on a pillow stack. weirdly helped more than the pill.
Stephen Craig
January 8, 2026 AT 19:43Long-term PPI use is a symptom of a broken healthcare system.
We prescribe drugs instead of asking why the stomach is reacting. We don’t teach nutrition. We don’t track outcomes. We just refill.
It’s not the pill that’s the problem. It’s the assumption that pills fix everything.
Connor Hale
January 9, 2026 AT 04:22I’ve been on PPIs for 7 years. I didn’t know any of this. My doctor never mentioned B12 or magnesium. I just got refills every 3 months.
Went in last week for a routine check-up. Asked if I still needed it. He paused. Said, ‘Actually… let’s try tapering.’
It’s not that he was negligent. It’s that no one talks about this. Not even the patients.
Thanks for the clarity.
Charlotte N
January 9, 2026 AT 10:51so i started taking otc prilosec because i had a weird burning after coffee… then i was on it for 2 years… i forgot i was even taking it… then i got dizzy and my hands tingled… went to the dr… b12 was half normal… i was like… wait… is this from the pill??
now i take a b12 shot every month… and i dont take the pill anymore… and my heartburn? gone… like… actually gone…
why does no one tell you this??
Rory Corrigan
January 10, 2026 AT 06:35the stomach is a temple… ppi’s are like putting a lock on the door… then wondering why the ghosts are still inside 😔
Jack Wernet
January 10, 2026 AT 15:55This is a remarkably well-researched and balanced overview of a critical public health issue that is too often overlooked by both patients and providers. The clinical nuances surrounding rebound acid hypersecretion, micronutrient deficiencies, and the distinction between association and causation in observational studies are presented with admirable precision.
It is imperative that clinicians engage in shared decision-making when prescribing long-term PPI therapy. The risks, while not universal, are sufficiently documented to warrant periodic reassessment. Furthermore, the emphasis on non-pharmacological interventions-dietary modification, sleep posture, and weight management-is not merely adjunctive; it is foundational.
Thank you for elevating this conversation beyond the realm of pharmaceutical marketing.
John Wilmerding
January 12, 2026 AT 04:04As a pharmacist with 18 years in clinical practice, I can confirm: 70% of long-term PPI users don’t need them. I’ve seen patients on PPIs since 2010 with no documented diagnosis-just ‘I had heartburn once and never stopped.’
Here’s what I tell my patients: You’re not weak for needing help. But you’re smart for asking if you still need it.
Always taper. Always test B12 and magnesium. Always try lifestyle changes first. And if your doctor says, ‘It’s fine to stay on it,’ ask: ‘When was the last time we reviewed why you’re on it?’
Most people are shocked when they realize they’ve been on it longer than their marriage.
Catherine HARDY
January 13, 2026 AT 10:44Did you know the FDA has been warned about PPIs since 2010? But the drug companies spent $1.2 billion lobbying to keep them OTC. They don’t want you to stop. They want you addicted.
And the ‘rebound’? That’s not a side effect-that’s a trap. They design it that way. You think you need it… so you keep buying.
Who benefits? The labs that test your B12. The hospitals that treat your kidney failure. The pharmacies that refill your script.
They don’t care if you live or die. They care if you keep paying.
Read the FDA’s yellow boxes. They’re not there for fun.
Siobhan Goggin
January 14, 2026 AT 13:35I’m from London and I’ve been telling my mates for years: if you’re taking heartburn pills every day, you’re probably eating too much cheese and too late. I switched to chamomile tea, stopped lying down after pasta, and haven’t touched PPIs in 18 months. My stomach’s happier. My wallet’s happier.
It’s not magic. It’s just… basic.
Vikram Sujay
January 16, 2026 AT 00:31This post is a masterclass in patient empowerment. In India, PPIs are sold over the counter without prescription, often bundled with painkillers at roadside pharmacies. Many patients take them for years without knowing the risks.
I now counsel my patients to ask three questions before refilling: Why did I start? Has my condition changed? What happens if I stop?
Most don’t have answers. That’s the problem.
Medication is not a permanent solution unless the root cause is addressed.
Jay Tejada
January 17, 2026 AT 03:53my cousin took ppi for 10 years. then she got kidney failure. doctors said ‘probably the ppi.’ she cried. she was 42. now she’s on dialysis.
she didn’t even know she had heartburn. she just took it because her mom said ‘it’s just acid.’
don’t be her.
Roshan Aryal
January 17, 2026 AT 04:40You Americans are so dramatic. In India, we take PPIs like aspirin. No one dies. No one gets kidney failure. You have too much time to worry about your stomach. We have real problems-power cuts, traffic, inflation.
Stop blaming the medicine. Blame your lazy lifestyle. Eat less junk. Move more. Stop watching Netflix after dinner. Then you won’t need pills.
This post is just fear-mongering for Westerners who think their bodies are fragile.