Gabapentin Alternative Comparison Tool
Compare different options based on your specific needs. This tool helps you understand which alternatives might work best for your condition and side effect tolerance.
Your Situation
Key Comparison
Neurontin, the brand name for gabapentin, has been a go-to prescription for millions dealing with nerve pain, seizures, and anxiety. But as side effects pile up - dizziness, weight gain, brain fog - people are asking: Gabapentin really the best option? Or are there safer, more effective alternatives out there?
What Gabapentin Actually Does
Gabapentin was originally developed as an anti-seizure drug in the 1990s. It works by calming overactive nerves in the brain and spinal cord. Today, it’s prescribed off-label for conditions like diabetic nerve pain, post-shingles pain (postherpetic neuralgia), restless legs syndrome, and even social anxiety. The FDA only approved it for seizures and nerve pain, but doctors use it widely for other issues because it’s cheap and widely available.
But here’s the catch: studies show gabapentin doesn’t work well for everyone. A 2023 review in The Lancet Neurology found that only about 30-40% of patients with nerve pain saw meaningful relief. And side effects? Nearly half of users report drowsiness, swelling, or trouble concentrating. For older adults, the risks climb even higher - falls, confusion, even kidney strain.
Top Alternatives to Gabapentin
If gabapentin isn’t cutting it, or if side effects are too much, here are the most commonly used and researched alternatives.
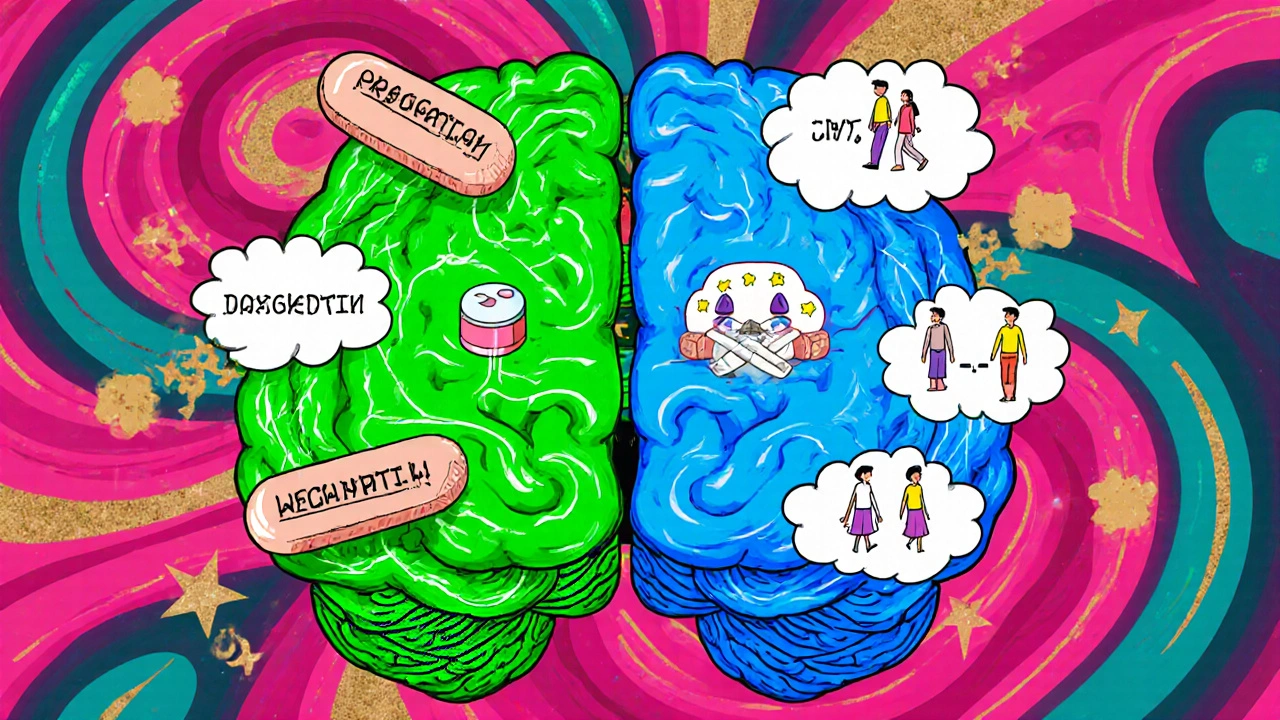
Pregabalin (Lyrica)
Pregabalin is gabapentin’s close cousin - same class of drug, same mechanism, but stronger and faster. It’s FDA-approved for the same conditions: nerve pain, seizures, fibromyalgia. But unlike gabapentin, pregabalin has more predictable absorption. You don’t need to take it three times a day. Once or twice is often enough.
Studies show pregabalin works better for some types of nerve pain. A 2022 trial in Pain Medicine found that 55% of patients on pregabalin reported at least 50% pain reduction, compared to 41% on gabapentin. But it’s not cheaper - Lyrica costs nearly triple the price of generic gabapentin. And it’s more likely to cause weight gain and dizziness.
Carbamazepine (Tegretol)
Carbamazepine has been around since the 1960s. It’s one of the oldest seizure meds, but it’s also a top pick for trigeminal neuralgia - that sudden, stabbing facial pain. For this specific condition, carbamazepine often beats gabapentin.
It’s not without risks. It can lower white blood cell counts, cause liver issues, and interact with dozens of other drugs. Blood tests are needed every few months. But for people who don’t respond to gabapentin, it’s a proven backup. Many neurologists in the UK start with gabapentin, then switch to carbamazepine if pain returns.
Topiramate (Topamax)
Topiramate is primarily used for epilepsy and migraine prevention. But it’s also used off-label for nerve pain and anxiety. What makes it different? It doesn’t cause weight gain - in fact, many people lose weight on it. That’s a big plus for those struggling with gabapentin-induced weight gain.
Side effects? Brain fog, tingling in hands and feet, trouble finding words. It’s not ideal for people who need sharp focus, like drivers or office workers. But for someone with chronic pain and obesity, topiramate might be the better trade-off.
Duloxetine (Cymbalta)
Duloxetine is an SNRI antidepressant - not an anti-seizure drug. But it’s FDA-approved for diabetic nerve pain and fibromyalgia. It works by boosting serotonin and norepinephrine, two brain chemicals that help regulate pain signals.
A 2021 meta-analysis in JAMA Neurology found duloxetine was just as effective as gabapentin for nerve pain, but with fewer drowsiness-related side effects. People on duloxetine reported better sleep quality and less mental fog. The downside? It can cause nausea, dry mouth, and sometimes increased blood pressure. And like all antidepressants, it takes 2-4 weeks to kick in.
Physical Therapy and Non-Drug Options
Medication isn’t the only path. For many, combining drugs with physical therapy, acupuncture, or mindfulness reduces reliance on pills entirely.
A 2024 NHS trial tracked 500 people with chronic back pain. Half got gabapentin. The other half got weekly physiotherapy plus cognitive behavioural therapy (CBT). After six months, both groups had similar pain relief - but the non-drug group had fewer side effects and lower dropout rates.
For people with restless legs or mild anxiety, simple changes help: regular walking, avoiding caffeine after 3 PM, magnesium supplements. These aren’t magic bullets, but they’re low-risk and often overlooked.
How to Choose the Right Alternative
There’s no one-size-fits-all answer. Your best option depends on your condition, your body, and your lifestyle.
- If you have facial nerve pain (trigeminal neuralgia) → Try carbamazepine first.
- If you gained weight on gabapentin → Topiramate or duloxetine might help.
- If you need quick, strong relief → Pregabalin works faster and more reliably.
- If you’re older or at risk of falls → Avoid gabapentin and pregabalin. Try duloxetine or non-drug options.
- If anxiety is your main issue → Duloxetine or CBT may be better than gabapentin, which has limited evidence for anxiety.
Always talk to your doctor before switching. Stopping gabapentin suddenly can cause seizures or severe withdrawal - even if you’ve only been on it a few weeks. Tapering down over weeks is essential.
What Doctors Are Saying Now
In the UK, the National Institute for Health and Care Excellence (NICE) updated its guidelines in early 2025. They now recommend gabapentin and pregabalin only as second-line treatments for nerve pain - after trying antidepressants like duloxetine or non-drug therapies.
Why? Because the long-term risks are clearer now. Studies show people on gabapentin for over a year have higher rates of falls, fractures, and cognitive decline. The NHS is pushing to reduce prescriptions, especially for older adults.
Many GPs now start with duloxetine or physical therapy. Gabapentin is still prescribed, but it’s no longer the default.
Real Stories: What Worked for Others
Marjorie, 68, from Bristol, had diabetic nerve pain for five years. Gabapentin helped at first, but she started falling. Her doctor switched her to duloxetine. Within six weeks, her pain dropped by 60%. She lost 8 pounds. No more dizziness.
James, 42, had post-shingles pain. Gabapentin gave him brain fog. He tried topiramate - the tingling was annoying, but his mind cleared. He now walks 5 miles a day and doesn’t need pills on weekends.
These aren’t outliers. They’re examples of people who found better fits after gabapentin didn’t work.
When to Stick With Gabapentin
That said, gabapentin still has a place. If you’re young, healthy, and respond well with minimal side effects - stick with it. It’s affordable. It’s been used safely by millions.
But if you’re experiencing side effects, or if it’s not working after 6-8 weeks, don’t just power through. Ask your doctor about alternatives. There’s a better option out there for you.
Is gabapentin addictive?
Gabapentin isn’t addictive like opioids or benzodiazepines, but it can cause physical dependence. Stopping suddenly can trigger anxiety, insomnia, or even seizures. Always taper off under medical supervision, even if you’ve only taken it for a few weeks.
Can I take gabapentin with alcohol?
No. Mixing gabapentin and alcohol increases drowsiness, dizziness, and risk of falls. It can also worsen depression or breathing problems. Avoid alcohol completely while on this medication.
Which is better: gabapentin or pregabalin?
Pregabalin works faster and more consistently than gabapentin, especially for nerve pain. But it’s more expensive and causes more weight gain. Gabapentin is cheaper and may be better for people who can tolerate its slower, less predictable effect. The choice depends on your budget, side effect tolerance, and how quickly you need relief.
Are there natural alternatives to gabapentin?
Yes, but they’re not direct replacements. Magnesium, alpha-lipoic acid, and acupuncture have shown modest benefits for nerve pain in studies. Physical therapy and CBT are proven to reduce pain and improve function without drugs. These work best alongside - not instead of - medical treatment, especially for severe pain.
How long does it take for gabapentin alternatives to work?
Pregabalin and carbamazepine often work within days. Duloxetine and topiramate take 2-6 weeks. Non-drug options like physiotherapy or CBT show results after 4-8 weeks. Don’t give up too soon - some alternatives need time to build up in your system or for your body to adapt.
Next Steps: What to Do Now
If you’re on gabapentin and it’s not working, or if side effects are getting worse:
- Write down your symptoms: What’s improving? What’s getting worse?
- Check your dosage - are you on the lowest effective dose?
- Ask your doctor about switching to duloxetine, topiramate, or pregabalin.
- Request a referral to physiotherapy or pain management if you haven’t already.
- Don’t stop gabapentin on your own. Ask for a tapering plan.
The goal isn’t just to reduce pain - it’s to live better. There are options. You just need to ask for them.




Dylan Kane
October 29, 2025 AT 02:07Okay but let’s be real - gabapentin is basically the pharmaceutical equivalent of a warm blanket you pretend is fixing your problems. I’ve seen so many people on it for ‘anxiety’ and they’re just zombies scrolling TikTok at 3 AM. Duloxetine? Way more human. No brain fog, just… calm. Also, why are we still prescribing this like it’s 2012?
KC Liu
October 29, 2025 AT 16:07Interesting how the article conveniently omits the fact that the FDA approved gabapentin for off-label use after being pressured by pharmaceutical reps who were paid millions to promote it. The real alternative? Stop letting Big Pharma dictate your pain management. The NHS guidelines? A distraction. They’re just trying to cut costs while you’re left with a broken body and a $200 monthly bill for duloxetine. Wake up.
Shanice Alethia
October 31, 2025 AT 15:57I HATE that people just say ‘try duloxetine’ like it’s some magical cure. I was on it for 3 months. Nausea so bad I threw up every morning. My doctor just said ‘it takes time.’ TIME? I lost 15 pounds and my job because I couldn’t focus. Gabapentin made me sleepy - duloxetine made me suicidal. So yeah, maybe stop giving people platitudes and start listening.
Sam Tyler
November 1, 2025 AT 06:29There’s a lot of nuance here that’s easy to miss. Gabapentin isn’t ‘bad’ - it’s just not universally effective, and we’ve overprescribed it because it’s cheap and easy. The real win isn’t swapping one pill for another; it’s building a holistic approach. Physical therapy isn’t ‘alternative’ - it’s foundational. CBT isn’t ‘fluffy’ - it’s neuroplasticity in action. And yes, magnesium helps, but only if you’re deficient. The key is personalized care, not a one-size-fits-all script. We need to stop treating pain like a math problem and start treating it like a person.
shridhar shanbhag
November 1, 2025 AT 11:03In India, we rarely see gabapentin prescribed for anxiety - it’s mostly for neuropathy or epilepsy. Even then, doctors prefer carbamazepine or pregabalin if available. But cost is a huge barrier. Most patients can’t afford Lyrica, so they suffer. The real issue isn’t the drug - it’s access. And yes, physiotherapy works, but where do you find a qualified therapist in a rural town? We need systemic change, not just individual swaps.
John Dumproff
November 2, 2025 AT 10:16Just wanted to say - if you’re reading this and you’re scared to talk to your doctor about switching meds, you’re not alone. I was too. But when I finally said, ‘This isn’t working for me,’ my doctor didn’t judge me. She said, ‘Let’s figure this out together.’ You deserve to feel better, not just numb. Take a breath. Write down your symptoms. Bring this post with you. You’ve got this.
Lugene Blair
November 3, 2025 AT 04:49STOP. Just stop. If you’re on gabapentin and you’re not getting better, you’re not weak. You’re not broken. You’re just not on the right tool for your job. I was on it for 2 years. Felt like I was underwater. Switched to topiramate - tingling? Yes. But I could think again. I started walking. I got my life back. You can too. Don’t let fear of change keep you stuck. You’re worth the effort.
William Cuthbertson
November 4, 2025 AT 05:25There’s something deeply human here - the way we’ve turned medicine into a gamble. We take pills not because they cure, but because we’ve lost faith in our bodies’ capacity to heal. Gabapentin doesn’t fix nerve pain - it muffles the signal. But what if the signal was never meant to be silenced? What if pain, however unbearable, is trying to tell us something? Physical therapy, mindfulness, even cold showers - these aren’t ‘alternatives.’ They’re invitations to re-engage with your own biology. The real question isn’t ‘which drug?’ - it’s ‘who do you want to be while you’re healing?’
Eben Neppie
November 4, 2025 AT 11:15Let me cut through the noise: pregabalin is superior in efficacy and pharmacokinetics. End of story. The fact that people still default to gabapentin is either ignorance or laziness. And don’t get me started on ‘natural alternatives’ - magnesium doesn’t reverse diabetic neuropathy. Acupuncture? Placebo with a massage. If you’re serious about pain management, you don’t wing it. You see a specialist. You get labs. You track outcomes. Stop listening to Reddit gurus and start working with a neurologist who knows what they’re doing.
Hudson Owen
November 6, 2025 AT 09:36While I appreciate the thorough analysis presented, I would respectfully suggest that the discussion be expanded to include emerging therapies such as transcutaneous electrical nerve stimulation (TENS) and low-dose naltrexone (LDN), both of which have demonstrated promising results in peer-reviewed literature for chronic neuropathic conditions. Additionally, the psychological component of pain perception - particularly in the context of trauma-informed care - warrants deeper integration into clinical decision-making frameworks.
Steven Shu
November 6, 2025 AT 14:03My dad was on gabapentin for 7 years. Started falling, got a hip fracture. Switched to duloxetine. He lost 10 pounds, slept better, and finally walked his granddaughter down the aisle. No magic. Just the right tool. If you’re struggling - ask for help. Don’t wait until you’re broken.
Dylan Kane
November 6, 2025 AT 20:55^ THIS. My mom’s story too. Gabapentin was her ‘easy fix’ until she couldn’t stand up. Duloxetine wasn’t perfect - but it let her live again. Stop romanticizing the ‘cheap’ option. Quality of life isn’t a budget line item.