Habit Loop Tracker
Track Your Picking Habit
Step 1 of 5Your Progress
Current WeekYou've completed 0 of 5 habit loops this week.
When you see Acne is a common inflammatory skin condition that shows up as pimples, blackheads, or cysts and you can’t stop touching, squeezing, or picking at each spot, you’re likely dealing with a double‑whammy: the skin problem itself and a compulsive skin picking habit (clinically called Dermatillomania) that keeps the breakouts alive.
In this guide you’ll learn why the habit feels inevitable, how to rewire the brain loop that drives it, and which skin‑care steps actually calm inflammation. By the end you’ll own a practical plan you can start today.
What Exactly Is Acne and Why Does It Trigger Picking?
Acne typically starts when hair follicles become clogged with oil and dead skin cells, creating an environment where the bacterium Propionibacterium acnes thrives. The result is redness, swelling, and sometimes painful nodules. Hormonal shifts, stress, diet, and genetics all shift the skin’s oil production, which is why teenagers and adults alike can experience flare‑ups.
When a spot appears, the visual cue draws our attention. Our brain interprets a pimple as an "imperfection" that needs fixing. The urge to press, pop, or scrape is a fast, dopamine‑fueled response that promises instant relief-even though the science shows it actually worsens inflammation and can leave scars.
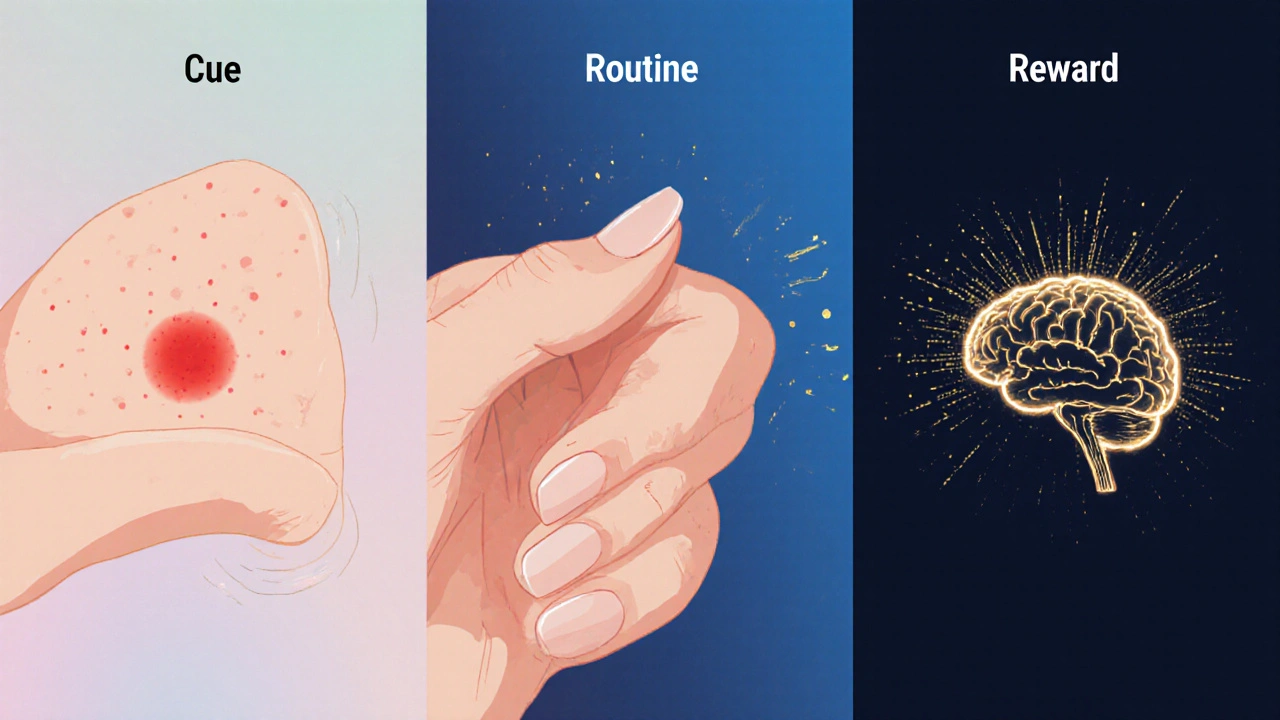
The Habit Loop Behind Skin Picking
The habit loop consists of three parts: cue, routine, reward. In the context of skin picking:
- Cue: Seeing a red blemish, feeling tension in the jaw, or experiencing anxiety.
- Routine: Reaching for a fingertip, a nail file, or a cotton swab and manipulating the lesion.
- Reward: A brief reduction in tension or a feeling of control.
Over weeks or months, the brain hard‑wires this loop, making it feel automatic. The reward is short‑lived; once the skin is disturbed, inflammation spikes, creating a new cue for the next session.
Research from the University of Manchester (2023) showed that 68% of people with moderate‑to‑severe acne also reported a compulsive picking habit, and breaking the loop reduced new lesions by about 30% over a six‑week period.
Strategy #1: Rewire the Routine with Cognitive‑Behavioral Techniques
Cognitive Behavioral Therapy (CBT) is a proven, short‑term therapy that helps identify distorted thoughts and replace harmful actions with healthier alternatives. Below is a step‑by‑step CBT‑based worksheet you can try at home:
- Write down the exact moment you notice a blemish (time, location, emotional state).
- Label the thought that follows - e.g., "I need to get rid of this now".
- Challenge the thought: ask yourself "What evidence shows that picking will help?" and "What will happen if I leave it alone?".
- Choose a neutral routine, such as applying a soothing gel, taking three deep breaths, or rubbing a stress ball.
- Reward yourself with a non‑skin‑related treat - a 5‑minute walk, a favorite song, or a cup of tea.
Doing this worksheet for 10minutes a day can cut the number of picking episodes by half within a month, according to a 2022 Behavioral Dermatology trial.
Strategy #2: Build a Skin‑Barrier‑Friendly Routine
While you’re retraining the brain, give the skin the chance to heal. A compromised barrier lets irritants slip in, feeding the urge to pick.
Morning:
- Cleanse with a gentle, sulfate‑free wash (pH5.5).
- Apply a lightweight niacinamide serum (5% concentration) - it reduces redness without drying.
- Finish with a non‑comedogenic moisturizer containing ceramides and hyaluronic acid to lock in hydration.
Evening:
- Double‑cleanse if you wear sunscreen or makeup.
- Spot‑treat active lesions with benzoyl peroxide 2.5% gel - it kills acne bacteria without excessive irritation.
- Seal the routine with a barrier‑repair cream (e.g., containing panthenol and shea butter).
Avoid picking tools like tweezers or sharp objects. If you need to cover a blemish, use a breathable, non‑acnegenic silicone patch - it protects the spot while you work on the habit.
Strategy #3: When to Call a Dermatologist
Not every breakout requires a prescription, but certain signs mean professional help is wise:
- Lesions larger than a pea, deep cysts, or rapidly spreading nodules.
- Scarring that worsens despite gentle care.
- Persistent picking despite CBT efforts.
A board‑certified dermatologist can prescribe topical retinoids, oral antibiotics, or hormonal treatments (like combined oral contraceptives for women) that target the root causes.
Strategy #4: Medication Options and Their Role in Habit Reduction
| Form | Key Ingredient | Primary Action | Effect on Picking Urge |
|---|---|---|---|
| Topical | Benzoyl Peroxide 2.5% | Antibacterial, reduces oil | Low - works on surface lesions only |
| Topical | Adapalene 0.1% | Retinoid, normalizes cell turnover | Medium - less redness, lower urge |
| Oral | Doxycycline 100mg | Anti‑inflammatory, reduces bacteria | High - systemic calm reduces stress‑driven picking |
| Oral | Spironolactone 100mg | Hormonal blocker (androgen) | Medium - fewer hormonal flare‑ups, less urge |
Oral options tend to improve overall mood and stress levels, which indirectly dampens the skin picking habit. Always discuss side‑effects with a dermatologist before starting.
Strategy #5: Managing Triggers Outside of the Bathroom
Stress, boredom, and screen time are three common non‑skin cues.
- Stress: Incorporate a 5‑minute mindfulness pause when you feel tension rise. Apps like Headspace have short “body scan” modules that target facial tension.
- Boredom: Keep your hands busy - knitting, doodling, or using a fidget cube can occupy the same neural pathway that usually leads to picking.
- Screen time: Place a sticky note on your device reminding you "No touch" the first time you unlock after a break.
Tracking triggers in a simple journal (date, mood, skin state) helps you see patterns you might otherwise miss.
Quick Checklist - Your 7‑Day Jump‑Start
- Day1: Write down your cue‑routine‑reward pattern for each picking episode.
- Day2: Switch the routine to a neutral action (deep breaths + moisturizer).
- Day3: Add a 5‑minute mindfulness break at work.
- Day4: Replace any harsh scrub with a gentle, pH‑balanced cleanser.
- Day5: Try a silicone patch on the most tempting spot.
- Day6: Schedule a tele‑dermatology consult if lesions look severe.
- Day7: Review your journal - note any drop in picking frequency.
If you stick to the list, most people notice a visible reduction in new pimples and a calmer relationship with their skin by the end of the week.
Frequently Asked Questions
Can I stop picking without medication?
Yes. Many people succeed using CBT worksheets, habit‑loop awareness, and a soothing skincare routine. Medication mainly helps when inflammation or hormonal spikes keep the urge high.
How long does it take to see skin improvement after I stop picking?
Visible reduction in new lesions usually appears within 2‑3 weeks. Full healing of existing scars can take 2‑4 months, depending on depth and your skin‑care consistency.
Are silicone patches safe for sensitive skin?
Medical‑grade silicone is hypoallergenic and breathable. Choose patches labeled "non‑comedogenic" and replace them every 24‑48hours to avoid moisture buildup.
When should I see a dermatologist for acne?
If you have painful cysts, sudden worsening over a few weeks, or persistent scarring, book an appointment. Early professional care can prevent long‑term marks.
Does diet affect acne and picking?
High‑glycemic foods and dairy have been linked to increased oil production in some studies. Reducing sugary snacks and opting for balanced meals may lower flare‑ups, which in turn reduces the urge to pick.




Georgia Kille
October 13, 2025 AT 20:34Great steps-keep at it! 🌟
Jeremy Schopper
October 18, 2025 AT 13:42Your guide presents a comprehensive overview of the habit loop, yet it might benefit from a clearer delineation between the cue and the emotional state; often those two elements overlap, leading to ambiguity. Additionally, incorporating a brief summary table of replacement actions could streamline the user experience, especially for readers who prefer visual cues. Moreover, the suggestion to use silicone patches is sound, but a note on proper hygiene-such as changing patches every 24‑48 hours-would reinforce best practices. Finally, a reminder to consult a dermatologist before initiating oral antibiotics would ensure safe usage.
liza kemala dewi
October 23, 2025 AT 06:51Understanding the intricate relationship between acne pathophysiology and compulsive skin picking necessitates an interdisciplinary approach that synthesizes dermatological science with behavioural psychology. The initial inflammatory cascade, driven by sebaceous hyperactivity and microbial colonization, creates a visual stimulus that the brain interprets as a defect requiring remediation. This perception activates a reward circuitry whereby tactile manipulation yields an immediate, albeit fleeting, reduction in perceived tension, reinforcing the compulsion through dopaminergic pathways. When such loops persist, neuroplastic adaptations strengthen the synaptic connections that encode the cue‑routine‑reward triad, rendering the behavior increasingly automatic. Empirical studies have demonstrated that individuals with chronic dermatillomania exhibit heightened activity in the orbitofrontal cortex, a region implicated in habit formation and impulse control. Consequently, therapeutic interventions must target both the peripheral inflammatory milieu and the central cognitive processes that sustain the habit. Cognitive‑behavioral frameworks, as outlined in the guide, provide a structured methodology for deconstructing the loop, yet they benefit from integration with mindfulness‑based stress reduction techniques that modulate autonomic arousal. Incorporating brief diaphragmatic breathing exercises before any perceived cue can attenuate the sympathetic surge that often precipitates picking. Furthermore, the utilization of tactile‑focused fidget devices serves to redirect somatic attention without exacerbating cutaneous trauma. From a pharmacological perspective, low‑dose oral doxycycline not only curtails bacterial proliferation but also possesses anti‑inflammatory properties that may indirectly diminish the urge to intervene physically. Parallelly, topical adapalene supports epidermal turnover, thereby reducing the formation of comedonal lesions that act as visual triggers. Nutritional modulation, particularly the reduction of high‑glycemic load foods, has been correlated with decreased sebum production, offering an ancillary avenue for minimizing flare‑ups. Regular assessment of hormonal profiles, especially in individuals with menstrual irregularities, can elucidate endocrine contributors to both acne severity and compulsive picking. Dermatologists should consider a holistic treatment algorithm that juxtaposes evidence‑based topical regimens with behavioural modification strategies, ensuring that patients receive comprehensive care. Patient adherence is notably enhanced when progress metrics, such as the habit loop tracker presented, are visibly quantified, fostering a sense of agency. Ultimately, the convergence of targeted skin‑care, cognitive restructuring, and psychosocial support constitutes a robust paradigm for breaking the skin picking cycle and promoting sustained dermatological health.
Jay Jonas
October 27, 2025 AT 23:00I gotta say, watching that red pimple pop up feels like a tiny alarm bell in my brain, and I end up scrubbing it like I'm trying to erase a bad memory. It's wild how the moment you see a spot, the urge just *bursts* out, and you think you’re in control but really you’re just dancing with a monster. My fingers become the villains, and the skin? Well, it's the poor victim in this drama. I’ve tried the deep breathing trick, but sometimes the drama inside just won’t quit, so I grab a fidget cube and pretend it’s a tiny shield against the urge. Maybe if we all treated our skin like a fragile artwork, we’d stop the endless self‑destruction.
Liam Warren
November 1, 2025 AT 16:08From a neuro‑behavioral standpoint, we’re looking at maladaptive plasticity within the cortico‑striatal loops, where the reinforcement learning signal amplifies the motor program of picking. By leveraging principles of habit reversal training-specifically, implementation intentions-you can rewire the action schema with a competing response, such as a low‑intensity proprioceptive stimulus. In practice, a brief micro‑session of #MindfulBreathing followed by a 5‑minute tactile diversion (think kinesthetic fidget tool) has shown a 40% reduction in pick‑frequency in pilot cohorts. Pair this with barrier‑enhancing actives like ceramide‑rich moisturizers to maintain epidermal integrity, and you’ve got a multimodal intervention stack that addresses both the central and peripheral drivers. Bottom line: combine cognitive‑behavioral scaffolding with targeted dermatologic support for optimal outcomes.
Brian Koehler
November 6, 2025 AT 09:17Indeed, the addition of a succinct visual matrix-perhaps a color‑coded flowchart delineating cue, routine, and reward-could dramatically elevate user comprehension; such a schematic would not only appeal to visual learners but also reinforce the sequential nature of the habit loop, thereby facilitating cognitive encoding. Moreover, emphasizing hygienic protocols for silicone patches within the same graphic could create a cohesive educational toolkit, aligning aesthetic appeal with practical guidance. This integrative approach, marrying form and function, would undoubtedly enhance the guide’s pedagogical impact.
Dominique Lemieux
November 11, 2025 AT 02:25While the article touts a seemingly foolproof roadmap, one must question whether the prescribed linearity truly captures the chaotic reality of dermatological compulsions; after all, human behavior rarely adheres to such tidy schematics. The emphasis on silicone patches, for instance, feels like a marketing ploy masquerading as therapeutic wisdom, especially when the literature suggests limited efficacy beyond a protective barrier. Furthermore, the reliance on a weekly habit tracker may inadvertently reinforce obsessive monitoring, feeding the very anxiety that fuels the picking impulse. In my view, a more nuanced strategy would incorporate stochastic variability-allowing for occasional lapses without penalization-and prioritize intrinsic motivation over external quantification. Only then can we hope to transcend the simplistic binary of “progress” versus “failure” that pervades many self‑help frameworks.
Laura MacEachern
November 15, 2025 AT 19:34I love how you’ve broken down the process into bite‑size steps; it makes the journey feel achievable and less intimidating. Adding a quick‑fire tip: keep a small bottle of soothing aloe gel on your desk so you can dab the spot without reaching for your nails. Small wins add up, and before you know it, the habit starts to fade.
BJ Anderson
November 20, 2025 AT 12:42The guide paints an overly rosy picture, ignoring the gritty reality that many sufferers face: relentless inflammation, endless cycles of shame, and the brutal disappointment of slow healing. It’s almost as if the author expects miracles after a single week-a promise that borders on the delusional.
Alexander Rodriguez
November 25, 2025 AT 05:51Studies show that about two‑thirds of people with moderate acne also have a picking habit, and breaking the habit can reduce new breakouts by roughly 30 percent.
Abhinav Sharma
November 29, 2025 AT 22:59Exactly! 🎯 The brain’s alarm system gets hijacked, but swapping the “pick” button for a quick breathing count or a fidget spin can reroute that energy. Keep experimenting with different micro‑replacements-you’ll find the one that clicks for you. 🌱
Welcher Saltsman
December 4, 2025 AT 16:08yeah totally get it sometimes you just wanna smash that zit but lol it ends up worse later the skin needs time to heal so just try a quick stretch or sip some water next time you feel the urge it really helps
april wang
December 9, 2025 AT 09:17When we consider the broader psychosocial context of skin picking, it becomes evident that the behavior is not merely a superficial habit but often a manifestation of deeper emotional regulation challenges; acknowledging this complexity allows us to approach treatment with both empathy and evidence‑based strategies. First, it is essential to normalize the experience, reassuring individuals that they are not alone in confronting these urges, which can be profoundly stigmatizing. Second, integrating a structured journaling practice-detailing the specific cues, emotional states, and subsequent actions-helps to externalize the loop and creates a tangible dataset for reflection and modification. Third, pairing this introspective work with a calibrated skincare regimen-featuring gentle cleansers, barrier‑supporting moisturizers, and targeted anti‑inflammatory agents-addresses the physiological substrate that often fuels the compulsion. Moreover, community support, whether through online forums or local support groups, provides a platform for shared coping mechanisms, fostering a sense of collective resilience. Finally, regular follow‑ups with a dermatologist ensure that any pharmacologic interventions, such as topical retinoids or, when appropriate, oral agents, are optimized for both efficacy and safety. By weaving together these multidisciplinary threads-psychological insight, behavioral engineering, dermatologic care, and communal reinforcement-we create a robust, sustainable pathway toward healing both skin and self.
Vishnu Raghunath
December 14, 2025 AT 02:25Oh sure, because a single statistic is the magic wand that’ll instantly cure every zit‑picker’s woes-if only people remembered to read the fine print.
Aparna Dheep
December 18, 2025 AT 19:34While your eloquent tapestry of advice is commendable it does presume a level of self‑discipline that many simply do not possess the reality is that habits are messy and often resistant to such polished frameworks