Antibiotics are one of the most important medical breakthroughs in history. Before they existed, even a simple cut or sore throat could turn deadly. Today, they save millions of lives every year. But not all antibiotics are the same. They don’t just kill bacteria randomly-they target specific parts of the bacterial cell, and each class works in a completely different way. Understanding how they work isn’t just for doctors. If you’ve ever been prescribed an antibiotic, knowing the basics helps you take it right and avoid misuse.
How Antibiotics Actually Work
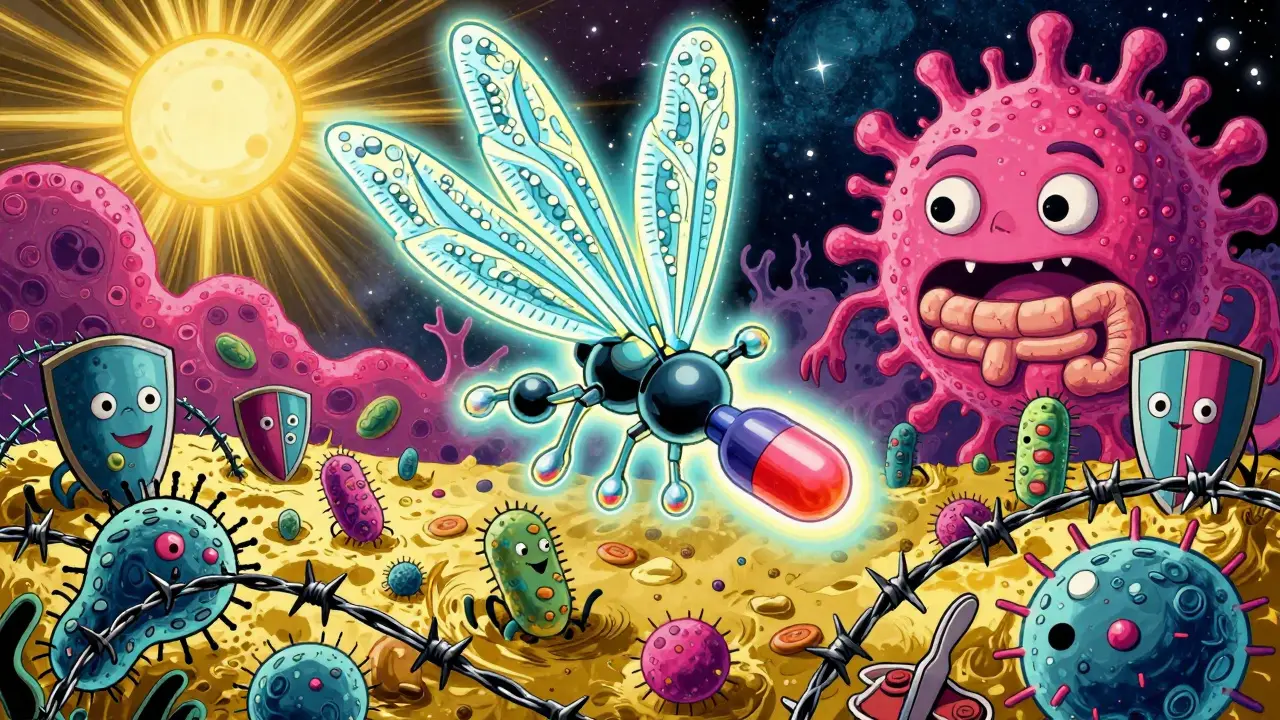
Antibiotics don’t work like a general cleaner. They’re more like precision tools. Some kill bacteria outright (bactericidal), while others just stop them from multiplying (bacteriostatic). Either way, they rely on differences between human and bacterial cells. Human cells don’t have cell walls, ribosomes like bacteria do, or the same DNA replication enzymes. Antibiotics exploit those differences. That’s why they can attack bacteria without wrecking your own cells-most of the time.
There are four main ways antibiotics do their job. Each targets a critical part of the bacteria’s survival system. If you understand these four, you understand nearly all antibiotics.
1. Disrupting the Cell Wall: Beta-Lactams and Glycopeptides
Bacteria have a tough outer shell called a cell wall. It’s like a protective suit that keeps them from bursting in your body’s watery environment. Beta-lactam antibiotics-like penicillin, amoxicillin, and cephalosporins-mimic a key building block in that wall. They sneak in and lock onto proteins called penicillin-binding proteins (PBPs). When those proteins can’t do their job, the wall falls apart. The bacteria swell up from internal pressure and pop. It’s a clean, efficient kill.
Penicillin was the first antibiotic ever used. Alexander Fleming found it in 1928, and by WWII, it was being mass-produced to treat wounded soldiers. Today, it’s still used for strep throat, ear infections, and skin infections. But bacteria have fought back. Many now make enzymes called beta-lactamases that cut up these drugs. That’s why doctors often pair penicillin with clavulanic acid (like in Augmentin), which blocks the enzyme.
Cephalosporins come in four generations. First-gen (like cefalexin) are good for skin and urinary infections. Second-gen (like cefuroxime) add coverage for some lung infections. Third-gen (like ceftriaxone) can handle more serious infections like meningitis. Fourth-gen (like cefepime) are broad-spectrum and used in hospitals for resistant bugs. Vancomycin, a glycopeptide, is used when penicillin fails-especially against MRSA. It’s given by IV because it doesn’t absorb well in the gut.
2. Stopping Protein Production: Macrolides, Tetracyclines, and More
Bacteria need proteins to survive. They build them using tiny machines called ribosomes. Antibiotics like macrolides (azithromycin, erythromycin) and tetracyclines (doxycycline) slip into these ribosomes and jam the assembly line.
Macrolides bind to the 50S subunit of the ribosome. They don’t stop protein building completely-they just make faulty ones. That’s enough to slow the infection down. Azithromycin is popular because it stays in the body for days after just one dose. It’s often used for pneumonia, bronchitis, and even some STIs like chlamydia.
Tetracyclines bind to the 30S subunit. They block the tRNA from attaching, so no new proteins can be made. Doxycycline is a workhorse. It treats acne, Lyme disease, and even some tick-borne illnesses. But it has downsides. It can make your skin super sensitive to sunlight. And if you give it to kids under 8, it stains their developing teeth yellow or gray. That’s why it’s avoided in children.
Aminoglycosides like gentamicin also hit the 30S ribosome, but they cause even more chaos. They make the ribosome read the genetic code wrong, so the bacteria produce broken, useless proteins. This is a bactericidal method. But these drugs are harsh. They can damage kidneys and hearing, especially with long use. They’re usually reserved for serious hospital infections like sepsis.
Linezolid, an oxazolidinone, is newer. It stops protein synthesis even earlier-right at the start. It binds to the 23S rRNA and prevents the ribosome from even forming. That’s why it’s used for tough infections like MRSA and VRE (vancomycin-resistant enterococcus). It’s one of the few antibiotics that can be taken orally or by IV, making it flexible for outpatient use.

3. Blocking DNA and RNA: Fluoroquinolones
Fluoroquinolones-like ciprofloxacin and levofloxacin-attack bacteria from the inside out. They go after two enzymes: DNA gyrase and topoisomerase IV. These enzymes are like molecular scissors that untangle DNA during replication. When fluoroquinolones block them, the DNA gets tangled and breaks. The bacteria can’t copy their genetic material, so they can’t multiply.
This class is powerful. It works well in the lungs, bladder, and even bones. That’s why it’s often used for pneumonia, urinary tract infections, and some types of food poisoning. But it’s not without risks. The FDA added black box warnings in 2022: fluoroquinolones can cause tendon ruptures, nerve damage, and even mental health side effects. Because of this, they’re now reserved for cases where safer options don’t work.
Resistance is growing fast. In 72 countries, more than half of E. coli strains are now resistant to fluoroquinolones. That’s why doctors are being told to avoid them unless absolutely necessary.
4. Other Important Classes: Sulfonamides, Nitroimidazoles, and More
Not all antibiotics fit neatly into the first three categories. Some use clever tricks.
Sulfonamides, like sulfamethoxazole (often paired with trimethoprim as Bactrim), block folate production. Bacteria need folate to make DNA and RNA. Humans get folate from food, but bacteria have to make it themselves. Sulfonamides mimic the building block, tricking the bacteria into using a fake version. This class is rarely used alone anymore because resistance is high. But it’s still effective for Pneumocystis pneumonia in people with weakened immune systems.
Metronidazole is another standout. It only works against anaerobic bacteria-bugs that don’t need oxygen. It’s used for stomach infections like C. diff, dental abscesses, and some pelvic infections. The drug gets activated inside these bacteria and shreds their DNA. But it has a nasty side effect: if you drink alcohol while taking it, you’ll get severe nausea, vomiting, and flushing. It’s called a disulfiram-like reaction. About 60-70% of people experience it.
Newer drugs like cefiderocol are pushing boundaries. It’s a cephalosporin, but it’s disguised as iron. Bacteria need iron to survive, so they actively pull it into their cells. Cefiderocol hijacks that system, sneaking past defenses that block other antibiotics. It’s used for life-threatening infections like carbapenem-resistant Klebsiella. Clinical trials showed a 75% cure rate where other drugs failed.
Why Misuse Is Dangerous
Antibiotics don’t work on viruses. Taking them for a cold, flu, or most sore throats won’t help-and it harms you. Every time you take an antibiotic unnecessarily, you’re giving bacteria a chance to adapt. Over time, they become resistant. That’s why the WHO calls antibiotic resistance one of the top global health threats.
Even when you need antibiotics, taking them wrong can cause problems. Stopping early because you feel better leaves behind the toughest bacteria. They survive and multiply. That’s how superbugs form. Taking the full course-even if you feel fine-is critical.
Antibiotics also wreck your gut microbiome. Studies show that after just one course, your gut bacteria can take up to a year to recover. That’s linked to higher risks of C. diff infections, which cause severe diarrhea and can be deadly. Narrow-spectrum antibiotics (like penicillin for strep throat) are better than broad-spectrum ones (like ciprofloxacin) because they’re more targeted.
What’s Next for Antibiotics?
The pipeline for new antibiotics is dry. Only 42 are in development globally, and just 16 target the WHO’s highest-priority pathogens. Drug companies don’t make much money from them. People use them briefly, then stop. Compare that to drugs for diabetes or high blood pressure, which people take for life. The UK tried a fix: paying £76 million a year for access to new antibiotics, no matter how many are used. It’s like a Netflix subscription for lifesaving drugs. If it works, other countries might follow.
Phage therapy-using viruses that eat bacteria-is in Phase III trials. It’s not a cure-all, but for multi-drug-resistant infections, it’s a lifeline. In the future, we may see more personalized antibiotic use, guided by rapid tests that tell doctors exactly which bug is causing the infection.
For now, the best tool we have is using antibiotics wisely. Know what class you’re taking. Understand why it was chosen. And never pressure a doctor for antibiotics if they say you don’t need them.
Can antibiotics treat viral infections like the flu or cold?
No. Antibiotics only work against bacteria. Viruses like the flu, common cold, or COVID-19 have completely different structures and replication methods. Taking antibiotics for a virus doesn’t help and can lead to side effects and antibiotic resistance. The CDC estimates that 30% of outpatient antibiotic prescriptions in the U.S. are unnecessary, mostly for viral illnesses.
Why do some antibiotics cause diarrhea or C. diff infections?
Antibiotics don’t just kill the bad bacteria-they also wipe out helpful ones in your gut. This disrupts the natural balance of your microbiome. When that balance is gone, a tough bacterium called Clostridioides difficile can take over. It produces toxins that cause severe diarrhea, fever, and stomach pain. Broad-spectrum antibiotics like clindamycin, fluoroquinolones, and cephalosporins carry the highest risk. Studies show people on broad-spectrum antibiotics are up to 17 times more likely to get C. diff than those on narrow-spectrum ones.
Are all antibiotics the same strength?
No. Antibiotics vary in spectrum (how many types of bacteria they cover) and potency. Narrow-spectrum antibiotics, like penicillin, target only certain bacteria-often Gram-positive ones like strep. Broad-spectrum antibiotics, like doxycycline or ciprofloxacin, hit a wide range, including both Gram-positive and Gram-negative bacteria. Broad-spectrum drugs are powerful but risk more side effects and resistance. Doctors choose based on the infection, patient history, and local resistance patterns.
Why can’t we just make new antibiotics faster?
Developing a new antibiotic is expensive and unprofitable. It costs over $1.5 billion to bring one to market, but the average annual revenue is only $17 million-far less than drugs for chronic diseases like diabetes or high cholesterol. Companies don’t get enough return on investment. Plus, new antibiotics are often held in reserve to slow resistance, meaning they’re rarely used. The FDA and WHO are trying to fix this with incentives, but progress is slow. Only 42 new antibiotics are currently in clinical trials worldwide.
What’s the difference between bactericidal and bacteriostatic antibiotics?
Bactericidal antibiotics kill bacteria directly-like beta-lactams (penicillin) and fluoroquinolones. Bacteriostatic ones stop bacteria from growing, letting your immune system finish them off-like tetracyclines and macrolides. In most cases, either works. But for people with weak immune systems (like those with cancer or transplants), bactericidal drugs are preferred because their bodies can’t fight effectively on their own.
How do doctors choose which antibiotic to prescribe?
Doctors use a combination of factors: the likely bug (based on symptoms and location), local resistance patterns, patient allergies, and whether the infection is mild or severe. For example, strep throat is usually treated with penicillin because it’s targeted, cheap, and effective. For a urinary tract infection, they might pick nitrofurantoin or trimethoprim-sulfamethoxazole. In hospitals, they often start with broad-spectrum drugs until lab results come back. Then they switch to something more specific. Procalcitonin blood tests are now used in some cases to tell if an infection is bacterial, helping avoid unnecessary prescriptions.
Antibiotics are powerful-but they’re not magic. Their effectiveness depends on how we use them. Every time you take one, you’re part of a global effort to keep these drugs working. Use them only when needed. Finish the full course. And never share them with others. Your health-and the world’s-depends on it.