Every time you take an antibiotic when you don’t need it, you’re not just helping yourself-you’re helping bacteria become stronger. That’s the hard truth behind the rise of antibiotic overuse. It’s not just about one person getting sick. It’s about entire communities losing the ability to treat simple infections. And right now, we’re losing the battle.
What Happens When Antibiotics Don’t Work Anymore?
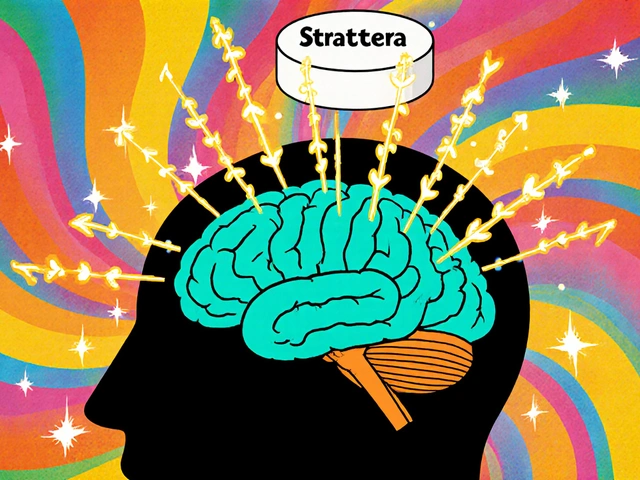
Antibiotics used to be magic bullets. A few pills, and a bad sore throat or urinary infection would vanish. Today, that’s no longer guaranteed. In 2023, one in six bacterial infections worldwide were resistant to standard antibiotics, according to the World Health Organization. That’s not a future threat-it’s happening now.When bacteria are exposed to antibiotics too often, they adapt. They evolve. Some survive the drug, multiply, and pass on their resistance. Over time, entire strains become untouchable by the drugs we once relied on. This isn’t science fiction. It’s clinical reality.
Take Escherichia coli, a common cause of urinary tract infections. In many parts of the world, 42% of these infections no longer respond to third-generation cephalosporins. For Staphylococcus aureus, nearly one in three cases are now methicillin-resistant (MRSA). And last-resort antibiotics like carbapenems? Their effectiveness is slipping fast. By 2035, resistance to these drugs could double compared to 2005 levels.
C. difficile: The Silent Consequence of Antibiotic Use
Every time you take an antibiotic, you’re not just killing the bad bacteria-you’re wiping out the good ones too. Your gut is home to trillions of microbes that keep you healthy. Antibiotics don’t care about that balance. They sweep through like a bulldozer.That’s where Clostridioides difficile, or C. difficile, comes in. This bacterium lives quietly in some people’s guts without causing harm. But when antibiotics kill off the competing bacteria, C. difficile takes over. It multiplies, releases toxins, and causes severe diarrhea, colitis, and sometimes death.
In the U.S. alone, C. difficile caused nearly half a million infections in 2017. While exact numbers for 2025 aren’t fully available, trends show it’s still climbing. The CDC confirms that antibiotic use is the single biggest risk factor for C. difficile infection. And here’s the kicker: the more antibiotics you take, the higher your risk. Even a single course can be enough.
Hospital patients are especially vulnerable. But it’s not just hospitals anymore. Community-acquired C. difficile cases have been rising for years. People who never set foot in a hospital are getting sick because they took antibiotics for a viral cold, a sinus infection that didn’t need them, or a mild ear infection that would have cleared on its own.
Why Are We Still Overusing Antibiotics?
You’d think doctors would know better. But pressure from patients, lack of quick diagnostics, and time constraints make it easy to reach for the prescription pad.Patients often walk in with a cough or runny nose and say, “Can you give me something for this?” They’ve been told antibiotics fix everything. Many don’t realize that antibiotics don’t work on viruses-cold, flu, most sore throats, and bronchitis are viral. Yet, in the U.S., about 30% of outpatient antibiotic prescriptions are unnecessary. In some countries, that number is even higher.
And it’s not just human medicine. About 70% of all antibiotics sold globally are used in livestock. Animals get them to grow faster or prevent disease in crowded, unsanitary conditions. Those antibiotics don’t disappear. They end up in our food, water, and soil. Resistant bacteria from farms can spread to humans through contact, consumption, or environmental contamination.
Even when doctors want to be careful, they’re often stuck. Without rapid tests to confirm whether an infection is bacterial or viral, they err on the side of caution. In low-resource settings, where labs are scarce, doctors have no choice but to guess-and guess wrong too often.
The Human Cost: More Deaths, Longer Hospital Stays, Higher Costs
Antibiotic resistance isn’t just a medical problem. It’s a human one.In 2019, resistant infections directly killed 1.27 million people worldwide. Another 4.95 million deaths were linked to them. That’s more than cancer. And by 2050, experts predict AMR could cause 10 million deaths a year-more than all cancers combined.
What does that look like in real life?
Imagine needing hip surgery. Before, you’d get a single antibiotic dose before the operation to prevent infection. Now, if the bacteria in your hospital are resistant, that dose might do nothing. You could end up with a post-surgery infection that won’t respond to any drug. Your recovery takes months. You need IV antibiotics with dangerous side effects. Or worse-you don’t recover at all.
Same with cancer treatment. Chemotherapy weakens your immune system. You rely on antibiotics to fight off infections. If those antibiotics don’t work, a simple fever could become fatal.
The economic toll is just as bad. The U.S. spends an extra $20 billion a year treating resistant infections. Globally, losses could hit $3 trillion annually by 2030. Hospitals are filling up with patients who should have been treated and sent home. Insurance premiums rise. Families lose income while caring for sick loved ones.
What’s Being Done-and Why It’s Not Enough
There are efforts to fix this. The WHO launched its Global Action Plan in 2015. Countries pledged to improve surveillance, reduce misuse, and invest in new drugs. Some progress has been made. In the U.S., hospital antibiotic use dropped 18% between 2012 and 2019.Then came COVID-19.
During the pandemic, antibiotic prescriptions soared-often without testing. Doctors were overwhelmed. Patients were scared. Hospitals relaxed rules. The progress we made? Gone. Resistant infections jumped 20% in U.S. hospitals between 2020 and 2022.
Meanwhile, the pipeline for new antibiotics is nearly dry. Drug companies aren’t investing because antibiotics aren’t profitable. A new cancer drug can earn billions. A new antibiotic? It’s used sparingly, for short periods, and only as a last resort. So companies don’t see the return.
Organizations like CARB-X have poured over $480 million into antibiotic research since 2016. They’ve funded 118 projects across 20 countries. But that’s a drop in the ocean. Only a handful of new antibiotics are in late-stage testing. And even if one works, it’ll take years to reach patients.
What You Can Do Right Now
You don’t need to wait for governments or drug companies to fix this. You have power too.- Don’t ask for antibiotics. If your doctor says it’s a virus, believe them. Ask what else you can do to feel better-rest, fluids, pain relievers.
- Take antibiotics exactly as prescribed. Never skip doses. Never save leftovers. Never give them to someone else.
- Never use antibiotics without a prescription. Online pharmacies, pet stores, or leftover pills from a past illness are not safe options.
- Ask about testing. If you have a persistent infection, ask if a rapid test can confirm whether it’s bacterial. Many clinics now have them.
- Choose meat raised without routine antibiotics. Look for labels like “no antibiotics ever” or “raised without antibiotics.” It reduces the spread of resistant bacteria from farms.
These steps aren’t just about you. They’re about protecting the people around you-your kids, your grandparents, your neighbor with diabetes. Every unnecessary antibiotic you avoid is one less chance for resistance to grow.
The Future Is Still in Our Hands
We’re at a turning point. If we keep going the way we are, we’ll return to a time when a scraped knee or a childbirth could kill you. When surgery becomes a gamble. When antibiotics become relics of the past.But we don’t have to accept that. The tools to stop this are already here: better diagnostics, smarter prescribing, public education, and responsible farming. What’s missing is the will to use them.
It’s not about fear. It’s about responsibility. Antibiotics saved millions. Now, we have to save antibiotics.
Can I get C. difficile from someone else?
Yes. C. difficile spores can survive on surfaces like doorknobs, toilets, and medical equipment for weeks. If someone with the infection doesn’t wash their hands properly, they can spread it. That’s why hospitals use special cleaning protocols and why handwashing with soap and water (not just hand sanitizer) is so important.
Are natural remedies a good alternative to antibiotics?
No. While some natural remedies may help with symptoms like sore throat or congestion, none can kill bacterial infections the way antibiotics do. Using them instead of proper medical care can delay treatment and allow infections to worsen. Always consult a doctor before skipping antibiotics when they’re truly needed.
Why don’t doctors test for every infection before prescribing antibiotics?
Many clinics don’t have fast, affordable tests for every possible infection. Blood or urine cultures can take days to return results. In urgent cases, doctors must treat based on symptoms. But more tests are becoming available-like rapid strep or flu tests-and asking for them helps push the system toward better practices.
Is antibiotic resistance only a problem in developing countries?
No. While resistance is growing fastest in regions with limited healthcare access, it’s a global problem. Resistant bacteria don’t stop at borders. Travel, food trade, and even air travel spread them. The WHO reports high resistance rates in Europe, North America, and Australia too. This is everyone’s issue.
If I’ve taken antibiotics before and they worked, why shouldn’t I use them again?
Because the bacteria causing your new infection might be different-and resistant. Also, your body’s microbiome changes over time. What worked last year might not work now, and could even trigger C. difficile. Always get a new diagnosis before taking antibiotics again.
What Comes Next?
The next step isn’t just about better drugs. It’s about changing how we think about infection. We need to treat antibiotics like a finite resource-like clean water or electricity. We use them wisely, or we lose them forever.That means supporting policies that fund antibiotic research, hold farms accountable for antibiotic use, and reward doctors who practice stewardship. But it also means each of us making smarter choices-every time we reach for a pill.
Antibiotics gave us modern medicine. Now, it’s our turn to protect them.



gent wood
November 15, 2025 AT 10:33Every time I see someone demand antibiotics for a cold, I cringe. I’ve seen family members lose months to C. diff after a simple sinus infection was treated with amoxicillin. It’s not just about the individual-it’s about the community. We’re all connected through this microbial web, and every unnecessary pill is a brick in the wall of resistance.
Sean Evans
November 16, 2025 AT 00:00Wow, another doomsday article. Let me guess-next you’ll tell us we should all stop breathing because air pollution is rising? Antibiotics aren’t magic, sure, but they’re not the apocalypse either. People get sick, they want to feel better, and doctors help. Stop acting like every prescription is a crime. Also, 70% of antibiotics go to livestock? Where’s your data? I’ve seen your sources-they’re all WHO propaganda.
Anjan Patel
November 17, 2025 AT 01:09Bro, I just got back from India, and let me tell you-antibiotics are sold over the counter at every chai stall. No prescription. No questions. My cousin took 10 courses in a year for fever, cough, even a headache. Now he’s in the hospital with MRSA. This isn’t just a Western problem. This is a global disaster waiting to explode, and no one’s doing anything. We’re all just waiting for the next pandemic to hit us while we still have pills in our cabinets.
Scarlett Walker
November 18, 2025 AT 18:15I love how this post doesn’t just scare us-it gives us real steps. I used to ask for antibiotics every time I had a sore throat, but now I just drink tea, rest, and wait. My doctor even high-fived me last time. Small changes matter. We can do this. 💪
Hrudananda Rath
November 18, 2025 AT 20:28One must observe, with considerable consternation, the alarming degeneration of medical praxis in the contemporary era. The casual dispensation of antimicrobial agents, devoid of diagnostic rigor, constitutes not merely negligence, but a metaphysical failure of the Hippocratic ethos. One is compelled to inquire: when did the populace begin to regard pharmaceuticals as confectionery?
Brian Bell
November 20, 2025 AT 17:44My grandma had C. diff after a single course of clindamycin for a tooth infection. She was fine for weeks, then boom-hospital for 3 months. Never took another antibiotic unless I was literally dying. And even then, I ask for a test first. Seriously, people-don’t be lazy. Your gut’s got feelings too.
Nathan Hsu
November 22, 2025 AT 03:38Let us not forget the cultural context: in many parts of Asia and Africa, antibiotics are seen as a sign of care, of being taken seriously. A doctor who doesn’t prescribe is perceived as uncaring. This is not ignorance-it is systemic mistrust. Until we fix the doctor-patient relationship, no amount of education will change behavior. We must heal the system, not just the patient.
Ashley Durance
November 23, 2025 AT 21:15Of course you’re blaming patients. But doctors are the ones writing the prescriptions. You think I don’t know people ask for antibiotics? I’m a nurse. I’ve seen the charts. Most doctors give them anyway because they’re scared of being sued if they don’t. The real problem is liability culture, not ignorance. Fix the system, not the people.
Scott Saleska
November 24, 2025 AT 13:12Wait, so if I had a UTI last year and took cipro, and now I have one again, I shouldn’t just take the leftover pills? But I know it’s the same thing… right? I mean, I’ve had it before. How is that different from taking ibuprofen for a headache that comes back? It’s the same body, same problem. Why is this so complicated?
Eleanora Keene
November 25, 2025 AT 11:34My sister’s a pediatrician. She told me the biggest shift in her practice? Parents now ask, "Can we try to hold off on antibiotics?" That’s new. Five years ago, it was "Give me something now." Progress is slow, but it’s happening. Keep sharing this stuff. We’re changing minds, one conversation at a time.
Ryan Anderson
November 27, 2025 AT 05:52Just took my last antibiotic last month for a sinus infection. Didn’t ask for it. Didn’t take it unless I had a fever for 5 days and green mucus. My doctor said "Good job." We need more people like this.