Medication Emergency Checker
This tool checks if your symptoms match critical red flags for life-threatening medication reactions. If any symptoms appear, call 999 immediately. This tool does not replace professional medical advice.
Check for Emergency Symptoms
Select any symptoms you're experiencing. If you have ANY of these, call 999 immediately:
Even if it feels like a cold. Airway closure requires immediate attention.
Can occur within minutes. Feeling of choking or voice change.
Sign of severe oxygen deprivation. Requires immediate action.
Especially if spreading fast or affecting mouth, eyes, or genitals.
Some medications trigger dangerous heart rhythms.
Organs not getting enough blood flow.
Hypertensive emergency - risk of stroke or brain bleeding.
Dry mouth, no urine for 12 hours, sunken eyes.
Possible internal bleeding, especially with blood thinners.
Even if never experienced before. Some drugs lower seizure threshold.
Starting a new medication can feel like rolling the dice. You take it because your doctor said so, but what if something goes wrong? Most side effects are mild - a little nausea, a dry mouth, maybe a headache. But some reactions can turn deadly in hours. Knowing the difference between a nuisance and a life-threatening emergency could save your life - or someone else’s.
What Counts as a Medication Emergency?
Not every weird feeling means you need an ambulance. But when your body reacts badly to a drug, timing is everything. The U.S. Food and Drug Administration defines a serious adverse drug reaction as one that causes death, hospitalization, disability, permanent damage, or birth defects. And these aren’t rare. More than 106,000 people in the U.S. die each year from adverse drug reactions - making them the fourth leading cause of death. The problem? Most people don’t know what to watch for. A 2023 study found only 42% of patients get clear instructions on when to call 911 versus when to call their doctor. That gap is deadly.Red Flags That Demand Immediate Emergency Care
These symptoms aren’t normal. They’re warning signs your body is in crisis. If you experience any of these after starting or changing a medication, call 999 or go to the nearest emergency department right away:- Difficulty breathing or wheezing - Even if it feels like a cold, if your airway is closing, every second counts.
- Swelling of the lips, tongue, or throat - This can happen within minutes of taking a pill. Your tongue might feel thick, your voice might change, or you might feel like you’re choking.
- Blue or gray lips or fingernails - This means your blood isn’t carrying enough oxygen. It’s a sign of anaphylaxis or severe respiratory failure.
- Sudden, severe rash with blistering or peeling skin - Especially if it spreads fast or affects your mouth, eyes, or genitals. This could be Stevens-Johnson Syndrome or toxic epidermal necrolysis - two rare but deadly skin reactions linked to antibiotics, anticonvulsants, and painkillers.
- Chest pain, rapid or irregular heartbeat (over 110 or under 50 bpm) - Some medications, like certain antibiotics or heart drugs, can trigger dangerous heart rhythms. Don’t wait to see if it passes.
- Very low blood pressure (below 90/60) with dizziness, fainting, or confusion - This isn’t just feeling lightheaded. It means your organs aren’t getting enough blood.
- High blood pressure over 180/120 with headache, slurred speech, weakness, or vision changes - This is a hypertensive emergency. It can cause stroke or brain bleeding.
- Uncontrollable vomiting or diarrhea with signs of dehydration - Dry mouth, no urine for 12 hours, sunken eyes, or extreme weakness. Some medications, especially antibiotics or diabetes drugs, can cause dangerous fluid loss.
- Severe abdominal pain radiating to your back - This could be a ruptured aneurysm or internal bleeding, especially if you’re on blood thinners like warfarin or rivaroxaban.
- Loss of consciousness or seizure - Even if you’ve never had one before. Some drugs lower the seizure threshold.
Common Medications That Trigger Life-Threatening Reactions
Some drugs are riskier than others. Here are the usual suspects:- Antibiotics - Penicillin and sulfa drugs cause the most severe allergic reactions. Even if you took them before without issue, allergies can develop anytime.
- NSAIDs - Ibuprofen, naproxen, and aspirin can trigger asthma attacks in some people and increase bleeding risk when taken with blood thinners.
- Warfarin and other blood thinners - Mixing these with common painkillers, antibiotics like ciprofloxacin, or even St. John’s Wort can spike your INR level dangerously fast - sometimes within 24 hours.
- Insulin and diabetes drugs - Too much can cause dangerously low blood sugar, leading to seizures or coma.
- Antidepressants and antipsychotics - Can cause serotonin syndrome: high fever, muscle rigidity, rapid heartbeat, and confusion. This is rare but deadly if untreated.
- Chemotherapy drugs - Often cause severe drops in white blood cells, leading to infections that can turn septic overnight.
And don’t forget supplements. St. John’s Wort, for example, can interfere with over 500 medications - including birth control, antidepressants, and heart drugs. Many people assume ‘natural’ means safe. It doesn’t.

When Is It Safe to Wait?
Not every odd feeling is an emergency. Mild side effects are common and usually harmless:- Light nausea or upset stomach (especially with antibiotics or painkillers)
- Headache or dizziness that fades after a few days
- Mild rash that doesn’t spread or blister
- Fatigue or dry mouth
If you’re unsure, ask yourself: Is this getting worse? Is it new? Did it start right after I changed my dose or added a new drug? If yes, don’t wait. Call your pharmacist or doctor. If you’re still unsure, err on the side of caution. Better to be checked than to regret waiting.
Why People Delay - And Why It’s Deadly
Many patients wait because they don’t recognize the symptoms. One Reddit user took amoxicillin and developed a rash and swelling but waited four hours, thinking it was just ‘an itchy allergy.’ By the time they got to the hospital, their throat was closing. They needed epinephrine and a breathing tube. Another common mistake: blaming symptoms on something else. A 35% misdiagnosis rate for anaphylaxis means people often think they’re having an asthma attack, panic attack, or food poisoning. But if you’re having trouble breathing and your face is swelling, it’s not anxiety - it’s anaphylaxis. And then there’s the polypharmacy problem. Nearly half of Americans over 65 take five or more medications daily. The more drugs you take, the higher your risk. One study found people on five or more meds have a 300% greater chance of a severe reaction than those on one.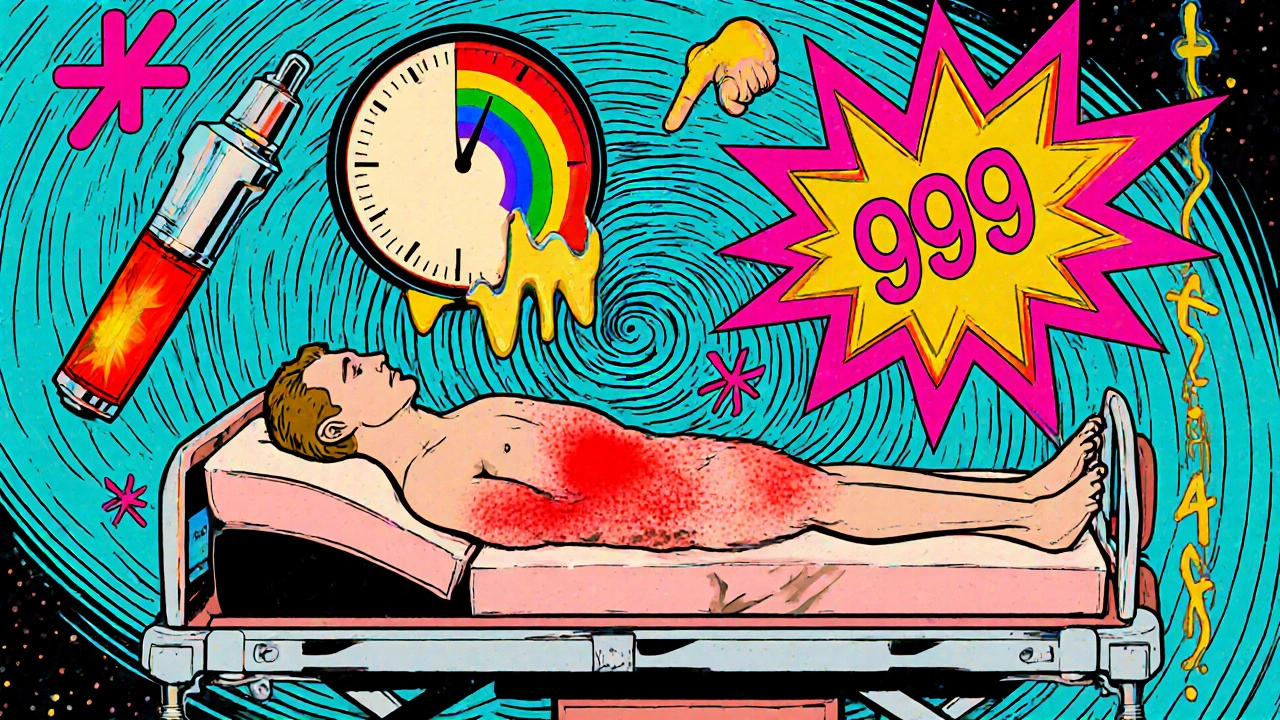
What You Can Do Right Now
You don’t have to wait for a crisis to act. Here’s how to protect yourself:- Keep a full list of everything you take - Prescription drugs, over-the-counter meds, vitamins, herbs, supplements. Bring it to every appointment.
- Ask your pharmacist - When they hand you a new script, ask: ‘What are the warning signs I should never ignore?’
- Know your emergency plan - Do you have an epinephrine auto-injector if you have a known allergy? Is it expired? Is your family trained to use it?
- Don’t ignore new symptoms after a dose change - 68% of severe reactions happen within 72 hours of starting or adjusting a medication.
- Use the FDA’s MedWatch program - Report any bad reaction, even if you’re not sure. It helps improve drug safety for everyone.
Pharmacists are your frontline defense. In the UK, community pharmacists now offer Medication Use Reviews - free consultations where they check for dangerous interactions. If your doctor didn’t mention it, ask for one.
What’s Changing in Medication Safety
The system is catching up. The FDA’s Sentinel Initiative now tracks 300 million patient records in real time to spot dangerous drug patterns within weeks - not years. AI tools are being tested to predict your personal risk of side effects based on your genes and medication history. By 2028, the U.S. medication safety tech market is expected to hit $4.7 billion. In the UK, NHS initiatives are expanding pharmacist-led medication reviews for high-risk patients, especially those on multiple drugs. These programs have already cut emergency visits for drug reactions by 18% in participating areas. But technology won’t fix what education misses. The real solution? Knowing what to look for - and acting fast.Can a medication reaction happen days after I start taking it?
Yes. While many reactions happen within hours - especially allergic ones - others can build up over days or weeks. For example, liver damage from certain antibiotics or statins might not show symptoms until after a week. Skin reactions like Stevens-Johnson Syndrome can take 1-3 weeks to develop. Always monitor for new symptoms, even if you’ve been on the drug for a while.
I have a rash from my medication. Should I go to the ER?
It depends. A mild, itchy, localized rash that doesn’t spread or blister is likely not an emergency - call your doctor. But if the rash is painful, blistering, peeling, or covering large areas of your body - especially if it’s in your mouth, eyes, or genitals - go to the ER immediately. These are signs of Stevens-Johnson Syndrome, a life-threatening condition.
What should I do if I think I’m having an allergic reaction?
If you have an epinephrine auto-injector (like an EpiPen), use it right away. Then call 999. Even if you feel better after the injection, you still need emergency care. Anaphylaxis can come back - sometimes worse - within hours. Never skip the ER after using epinephrine.
Can over-the-counter drugs cause serious reactions?
Absolutely. Ibuprofen, naproxen, and even high-dose acetaminophen can cause liver damage, internal bleeding, or severe allergic reactions. Many people assume OTC means safe, but taking too much - or mixing them with other drugs - can be deadly. Always check labels and talk to your pharmacist before combining medications.
I’m on blood thinners. What symptoms should I watch for?
Watch for unusual bruising, nosebleeds that won’t stop, blood in your urine or stool, or sudden severe headaches, dizziness, or weakness - these could mean internal bleeding. If you’re taking warfarin, avoid NSAIDs like ibuprofen, and limit alcohol. Always tell your doctor about any new medications or supplements, even herbal ones like ginger or ginkgo, which can increase bleeding risk.
How can I tell if a symptom is from my medication or something else?
Look at timing. Did the symptom start within hours or days of a new drug or dose change? If yes, it’s likely related. Also, ask yourself: Is this symptom new? Is it getting worse? Does it match known side effects of the drug? When in doubt, contact your pharmacist. They’re trained to spot these patterns.
Is it safe to stop a medication if I think it’s causing problems?
Never stop a prescription drug suddenly without talking to your doctor - especially for blood pressure, seizure, or mental health meds. Stopping abruptly can cause dangerous withdrawal symptoms or rebound effects. Instead, call your doctor or pharmacist. They can help you decide whether to stop, switch, or adjust the dose safely.





Bob Martin
October 29, 2025 AT 23:25Let me guess - you think if you just ignore the swelling it'll go away like a bad Tinder date? I've seen people wait for 'it to pass' and end up on a ventilator. The list in this post? That's not a suggestion. That's a survival checklist. Stop overthinking and call 911.
Sage Druce
October 31, 2025 AT 22:11I'm so glad someone finally put this out there in plain language. My mom took a new antibiotic and got a rash. She thought it was 'just dry skin' and waited three days. By then she was in the ICU. Don't be like my mom. If something feels wrong, trust it. You know your body better than any algorithm.
Emil Tompkins
November 2, 2025 AT 19:46Wow wow wow - so now we're all supposed to panic every time we get a headache after taking ibuprofen? I mean really. I've been on 12 different meds since 2018 and I'm still standing. Maybe the real emergency is the fear-mongering? This post reads like a pharmaceutical ad disguised as medical advice. Chill out. Your body's not a bomb.
Kevin Stone
November 3, 2025 AT 01:32It's not fear-mongering, it's education. People don't die because they're scared - they die because they're ignorant. The FDA stats are real. The symptoms listed? They're not opinions. They're clinical criteria. If you're going to take a drug, you owe it to yourself to know the risks. Ignorance isn't bravery. It's negligence.
Bart Capoen
November 3, 2025 AT 22:49my cousin took a new blood pressure med and got this weird tingling in her fingers. she thought it was nerves. turned out it was a reaction to the potassium additive. she ended up in the hospital for 5 days. i wish someone had told her to just call the pharmacist first. they're literally paid to answer this stuff. no need to panic, but don't ignore it either.
Cecil Mays
November 4, 2025 AT 22:19THIS. So many people think 'natural' = safe. St. John's Wort messing with birth control? That's not a myth. That's a pregnancy waiting to happen. I used to work ER. Saw too many cases where people thought 'it's just a supplement' and ended up in cardiac arrest. Knowledge saves lives. Share this. Please.
Tyler Mofield
November 6, 2025 AT 16:17While the intent of this article is commendable, the conflation of statistically significant adverse drug reactions with anecdotal fear-based narratives undermines its scientific credibility. The data presented, while alarming, lacks proper contextualization regarding incidence rates, confounding variables, and population denominators. One must exercise epistemological caution when interpreting pharmacovigilance reports.
Patrick Dwyer
November 8, 2025 AT 15:18Tyler, I get what you're saying about data, but most people don't have a PhD in pharmacology. They need clear, actionable info. This post gives them that. The FDA's numbers aren't theoretical - they're real people. Your jargon won't save someone with a swelling tongue. This? This will. Keep it simple. Save lives.
Shilah Lala
November 8, 2025 AT 22:23Oh wow. So now I'm supposed to run to the ER every time I feel like I might be dying? Because I had a headache after taking Advil? I'm just gonna sit here with my tea and let my body do its thing. I'm not paying for a $1500 ER visit because my anxiety is louder than my common sense.
Gary Fitsimmons
November 9, 2025 AT 06:38I hear you. I used to be like that too. But when my neighbor's kid got a rash after amoxicillin and didn't go to the hospital, he lost his airway. They had to cut his throat to save him. That's not fear. That's fact. You don't have to panic. But you do have to know the signs. Your body isn't lying to you. Listen.
Stuart Palley
November 10, 2025 AT 11:28Just one sentence: I took a new painkiller, got a rash, thought it was nothing, waited 12 hours, and woke up in the ER with my skin peeling off. Don't be me.