Parkinson's Protein Calculator
How to Use This Calculator
1 Enter your weight and meal details.
2 Calculate protein content per meal.
3 Check if your morning meals stay under 7g protein.
4 See how much protein you should have for dinner.
Meal Guidelines
Breakfast & Lunch: Keep protein under 7g per meal for best results.
Dinner: Should contain 80-85% of your daily protein intake.
Example: 70kg person needs 45-55g daily protein. Breakfast/Lunch should be under 7g each. Dinner should be 36-47g.
Results
Important Note
Your goal should be to keep breakfast and lunch under 7g of protein each. If you have more than 7g in either meal, your levodopa may not work as effectively.
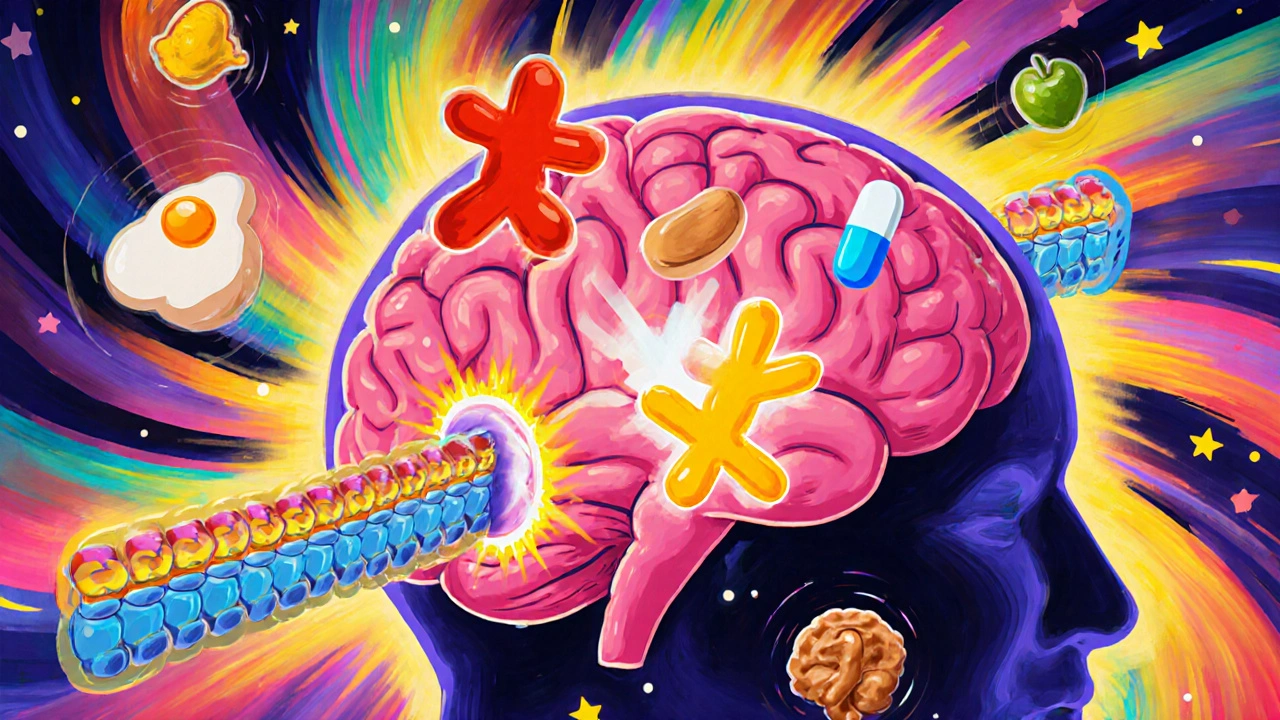
For people with Parkinson’s disease taking levodopa, what you eat isn’t just about nutrition-it can make the difference between moving freely and being stuck in an "off" period. This isn’t speculation. It’s a well-documented, physiological battle happening inside your body every time you eat a meal rich in protein. The amino acids from that chicken, egg, or beans are competing with your medication for the same doorway into your brain. And if you don’t know about it, your symptoms can get worse without any change in your drug dose.
Why Protein Blocks Levodopa
Levodopa doesn’t just float into your brain. It needs a specific transporter, called LAT1, to cross the blood-brain barrier. That same transporter also carries large neutral amino acids (LNAAs)-the building blocks of protein. Think of it like a single-lane bridge. When your body digests a steak or a cup of lentils, it floods your bloodstream with leucine, isoleucine, phenylalanine, and other LNAAs. Suddenly, there’s a traffic jam. Levodopa gets stuck waiting. Its absorption drops by 25-40%. The peak level in your blood is delayed by up to 90 minutes. And the result? Your medication takes longer to work-or doesn’t work at all.This isn’t something that happens right away. Most people don’t notice it until they’ve been on levodopa for 8 years or more. By then, the brain’s ability to store dopamine is fading, and every little drop in levodopa delivery becomes noticeable. Studies show 40-50% of long-term users experience this. You might feel fine in the morning, then suddenly stiffen up after lunch. That’s not your disease getting worse-it’s your protein.
What Counts as a "High-Protein" Meal?
You don’t need a giant steak to cause trouble. Just 10 grams of protein in a single meal can start to interfere. That’s about:- One large egg (6g)
- Two tablespoons of peanut butter (8g)
- Half a chicken breast (20g)
- One cup of cooked kidney beans (15g)
A typical lunch with grilled salmon, quinoa, and yogurt can easily hit 30-40 grams. That’s more than enough to knock your levodopa out of sync. Research shows meals with over 20 grams of protein can reduce levodopa bioavailability by up to 40%. And it’s not just the amount-it’s the timing. If you take your pill right before or after a protein-heavy meal, the competition is at its worst.
The Three Dietary Strategies That Actually Work
There are three main ways doctors and dietitians help patients manage this. Not all work for everyone, but one stands out.1. Low-Protein Diet (LPD)
This approach cuts total daily protein to 0.6-0.8 grams per kilogram of body weight. For a 70kg person, that’s about 45-55 grams total per day. Sounds simple? It’s not. Most people eat 70-100 grams daily. Cutting it down means giving up meat, dairy, eggs, legumes, and even bread. The result? Many lose weight, get weak, or develop deficiencies in vitamin B12 and iron. Studies show 31% of people on strict LPD lose more than 5% of their body weight in six months. It’s effective for some, but hard to sustain-and dangerous if you’re already underweight.2. Protein Redistribution Diet (PRD)
This is the most effective strategy-and the one most recommended by movement disorder specialists. Instead of cutting protein, you move it. You eat almost all your daily protein at dinner. During the day, you keep meals under 7 grams of protein. That means breakfast and lunch become low-protein: oatmeal with fruit, rice cakes with jam, vegetable soup, pasta with tomato sauce, or a smoothie made with low-protein milk substitute.Why does this work? Because levodopa works best during the day when you need to move. At night, you’re not walking, dressing, or cooking. So if your protein is hitting your system while you sleep, it doesn’t interfere with your mobility. Research shows PRD reduces "off" time by over 100 minutes per day and adds 30 minutes of smooth, controlled movement. One patient on Reddit reported gaining 2.5 extra hours of reliable mobility after switching to PRD under dietitian supervision.
PRD works best for people in Hoehn & Yahr stages 3-4, meaning they’re experiencing clear motor fluctuations. Studies show 60-100% of fluctuators respond to it. It’s more effective than low-protein diets alone-35% better at reducing symptoms.
3. Low-Protein Products (LPP)
These are specialty foods: low-protein bread, pasta, and flour. They help people stick to PRD by letting them eat familiar meals without the protein load. But here’s the catch: only 22% of users say they’re satisfied with them. They’re expensive, hard to find outside Europe and North America, and often taste off. They help, but they’re not a magic fix.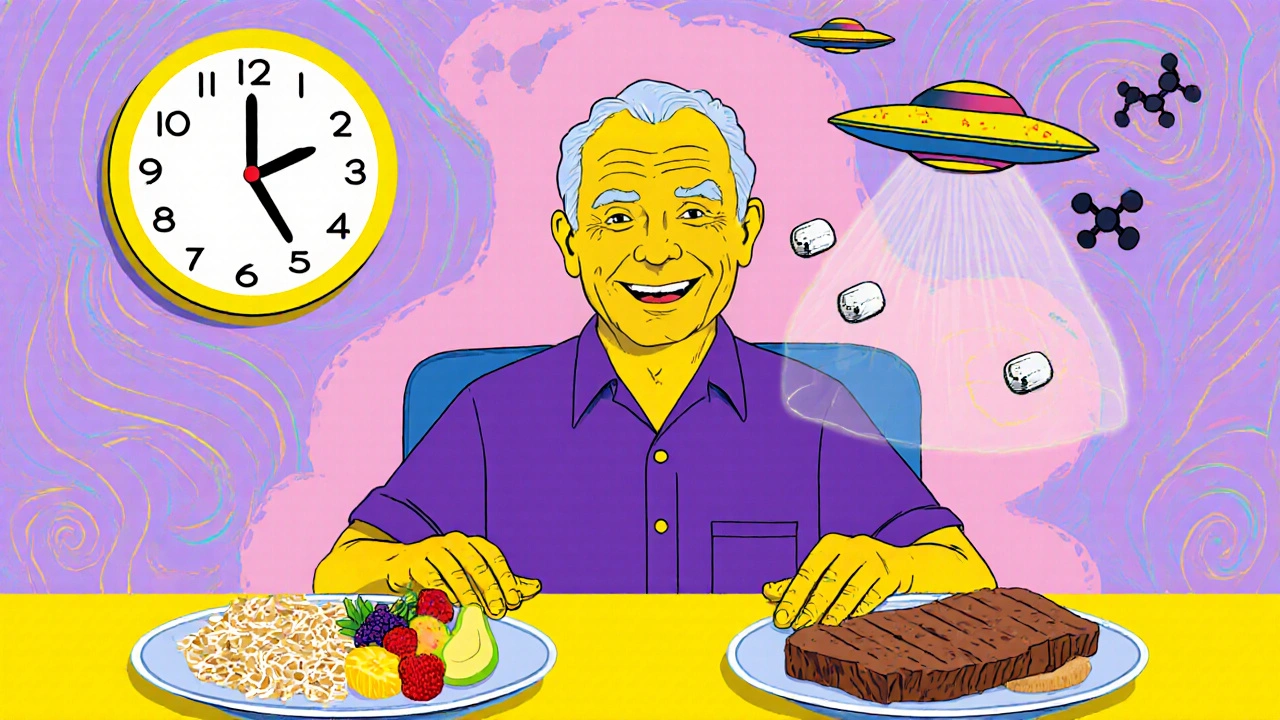
Timing Matters-But It’s Not Perfect
Some doctors suggest taking levodopa 30-60 minutes before meals. It sounds logical. And for some people, it works. But it’s inconsistent. Why? Because digestion varies. If your stomach empties slowly (common in Parkinson’s), the medication might still be sitting there when protein arrives. Studies show success rates range from 30% to 65%. It’s not reliable enough to rely on alone.What works better? Take levodopa 45 minutes before breakfast. That’s the most successful timing strategy reported by users. If you take it on an empty stomach, then wait 30-45 minutes before eating, you give levodopa a clear shot at the transporter. Many patients report this simple change improves their morning mobility.
Who Should (and Shouldn’t) Try This
Not everyone needs to change their diet. Only 40-50% of people on levodopa have a clinically significant interaction. If you’re still moving well, your symptoms are stable, and you don’t have "off" periods after meals-you probably don’t need to change anything.But if you’re noticing:
- Medication works fine in the morning but fades after lunch
- You have unpredictable "off" episodes tied to meals
- You’ve been on levodopa for 8+ years
Then it’s time to consider PRD.
But if you’re underweight (BMI under 20), have lost weight recently, or struggle to eat enough, don’t cut protein. You risk malnutrition. In those cases, doctors may adjust your levodopa dose instead-often reducing it by 15-25% if PRD is working, because you’re getting more consistent absorption.

Real-Life Challenges: Why People Quit
The biggest problem isn’t science-it’s life. Sixty-eight percent of people who start PRD quit within a year. Why?- Family dinners become impossible
- Going out to eat feels like a minefield
- Food becomes boring and restrictive
- Social isolation spikes-58% of users say dietary rules hurt their relationships
One woman in Bristol told her dietitian: "I stopped going to my daughter’s birthday parties because I didn’t want to eat just salad while everyone had cake and roast chicken. I missed out on those moments."
But here’s the good news: when dietitians tailor plans to cultural preferences, adherence jumps 40%. A person who eats rice and beans daily doesn’t need to switch to low-protein pasta. They can swap beans for tofu (lower protein) or reduce portion size. A Mediterranean diet can still work-it just needs tweaking.
How to Get Started
Don’t try this alone. Self-management fails more often than it succeeds. The Parkinson’s Foundation found that 78% of people who work with a dietitian achieve better symptom control than those who go it alone.Here’s how to begin:
- Track your food and symptoms for one week. Note what you eat, when you take levodopa, and when you feel "off."
- See a registered dietitian who specializes in Parkinson’s. They’ll help you calculate your protein needs and design a PRD plan.
- Start with breakfast and lunch. Aim for under 7g protein per meal. Use apps like MyFitnessPal to track.
- Save 80-85% of your daily protein for dinner.
- Take levodopa 45 minutes before breakfast and lunch.
- Reassess after 3-4 weeks. Do you have more "on" time? Less stiffness?
It takes 2-3 months to get comfortable. But for many, the payoff is huge: more hours of control, less unpredictability, and better quality of life.
What’s Next? The Future of Protein Management
Scientists are working on smarter solutions. One promising trial (NCT04876321) is testing "protein pacing"-giving small amounts of protein every few hours to keep amino acid levels steady, so they don’t overwhelm the transporter. Early results show 68% of participants respond well-and adherence is much higher than with PRD.Another idea? Medications that bypass the LAT1 transporter entirely. If developed, they could make dietary restrictions a thing of the past.
For now, though, the best tool we have is knowledge. Knowing that your protein is fighting your medication isn’t about restriction-it’s about reclaiming control. You don’t have to give up food. You just need to rearrange it.
Does all protein affect levodopa the same way?
No. All dietary proteins break down into large neutral amino acids (LNAAs), which compete with levodopa. So whether it’s chicken, beans, tofu, or dairy, the effect is the same. The key is the total amount of protein per meal, not the source. One cup of lentils and a chicken breast both contain around 15-20g of protein-and both can interfere.
Can I still eat meat if I’m on levodopa?
Yes, but timing matters. You can eat meat, fish, or eggs-but save them for your evening meal. Keep breakfast and lunch low in protein (under 7g). This way, your medication works when you need it most, and you still get the protein your body needs for muscle and repair. Many people find they can enjoy a nice steak at dinner without affecting their daytime mobility.
How long does it take to see results from a protein redistribution diet?
Most people notice improvements within 2-4 weeks. The biggest changes are often in morning mobility and fewer unpredictable "off" periods after meals. Full stabilization usually takes 6-8 weeks. Keep a symptom diary to track progress. Some patients report gaining 1-3 extra hours of good "on" time per day.
Is it safe to cut protein long-term?
Only if done carefully. Cutting protein too much can lead to muscle loss, weakness, and deficiencies in vitamin B12, iron, and zinc. That’s why protein redistribution (PRD) is preferred over strict low-protein diets. PRD keeps your total daily protein at healthy levels-it just shifts it to dinner. Always work with a dietitian to ensure you’re meeting your nutritional needs.
What if I’m underweight or losing weight?
Don’t restrict protein. Weight loss is a serious risk in Parkinson’s, and cutting protein can make it worse. Instead, talk to your doctor about adjusting your levodopa dose or timing. Some people benefit from taking smaller, more frequent doses of levodopa throughout the day, even with meals. Your care team can help you find a balance between mobility and nutrition.
Can I use protein shakes or supplements?
Avoid standard protein shakes during the day-they’re packed with amino acids that block levodopa. If you need extra calories or nutrition, look for low-protein nutritional supplements designed for Parkinson’s patients. Some brands make shakes with under 2g of protein per serving. Always check the label and ask your dietitian for recommendations.
If you’ve been struggling with unpredictable symptoms and think protein might be the culprit, you’re not alone. This isn’t about giving up food-it’s about taking back control of your movement. With the right plan, you can eat well, stay strong, and keep moving.




Ankit Right-hand for this but 2 qty HK 21
November 15, 2025 AT 11:34Bro this is just western medicine nonsense. In India we’ve been eating dal and roti with our meds for 50 years and no one’s stuck in an "off" period. You think your protein is the problem? Nah. It’s your weak willpower and overmedicated brain. Try yoga instead.
Oyejobi Olufemi
November 15, 2025 AT 21:13Let me dissect this with the precision of a neurophilosopher… You see, the LAT1 transporter isn’t merely a biological gate-it’s a metaphysical crossroads where the material and the immaterial collide. Protein isn’t the enemy; it’s the mirror reflecting our collective denial of mortality. The body isn’t failing-it’s whispering. And we? We’re too busy counting grams to hear the silence between the neurons.
Also, your "PRD" is just capitalism repackaging hunger as a lifestyle brand. Who profits? Big Pharma. Who suffers? The poor who can’t afford low-protein pasta. This isn’t medicine-it’s a luxury performance.
Daniel Stewart
November 16, 2025 AT 19:50Interesting framing. I wonder if the cultural context of meal timing plays a role here. In the UK, dinner is often the largest meal, and it’s typically eaten later-around 7 or 8 PM. That might naturally align with PRD without needing to restructure the whole day. The real issue isn’t the science-it’s the assumption that everyone eats like an American. My grandmother took levodopa with her Sunday roast and never had an off period. Maybe it’s not the protein-it’s the timing of the medication relative to digestion, not the protein itself.
Also, the study sample sizes seem small. 31% weight loss? That’s alarming, but from how many people? I’d like to see the raw data.
Latrisha M.
November 18, 2025 AT 11:15Thank you for writing this. Clear, evidence-based, and compassionate. I’m a neurology dietitian and I’ve seen PRD transform lives. One patient went from 12 hours of "off" time to 3. She cried when she could tie her shoes again without help. The key is personalization-not restriction. Work with a specialist. Track your symptoms. Don’t guess. And if you’re underweight, don’t cut protein-adjust your meds. You deserve to move, eat, and live.
Jamie Watts
November 20, 2025 AT 08:05Look I’ve been on levodopa for 12 years and I eat steak for breakfast every day and I’m fine so your whole theory is garbage. This is just another diet fad pushed by people who hate meat. You think your body is some delicate machine? Nah it’s a tank. If you’re having off periods it’s because you’re not taking enough. Take more. Or get off the meds. Simple. Stop overcomplicating food. Eat what you want. Move your body. End of story.
John Mwalwala
November 22, 2025 AT 06:26Wait… have you considered that this isn’t about protein at all? The LAT1 transporter is a decoy. Big Pharma introduced synthetic amino acid analogs into the food supply in the 90s to create dependency on levodopa. The real issue is glyphosate in soy and corn-those molecules bind to the transporter and block levodopa on purpose. That’s why PRD works-it’s not timing, it’s eliminating processed foods. Check your labels. If it’s not organic and non-GMO, it’s a weapon. Also, the FDA knows. They’ve been quiet since 2017. That’s why they’re pushing low-protein pasta-it’s a distraction. You’re being manipulated.
Deepak Mishra
November 23, 2025 AT 20:47OMG I JUST REALIZED WHY I’VE BEEN STUCK IN OFF PERIODS AFTER LUNCH!!! I’VE BEEN EATING CHICKEN CURRY WITH RICE EVERY DAY!!! 😭 I’M SO STUPID I DIDN’T KNOW PROTEIN WAS THE CULPRIT!!! I’M GOING TO SWITCH TO JUST CHAPATI AND JAM FOR BREAKFAST NOW!!! 🙏🙏🙏 I’M TELLING EVERYONE ON WHATSAPP!!! 🤯🤯🤯
Rachel Wusowicz
November 24, 2025 AT 05:33They’re not talking about the real threat: the food industry’s collusion with pharmaceutical companies to sell you low-protein bread at $12 a loaf while you’re told to avoid beans. I’ve seen it. I’ve seen the patents. The "low-protein pasta"? It’s made from corn syrup and industrial fillers. The real solution? Homemade rice noodles with lentil broth-no additives, no corporate logos. But you won’t find that in the studies. Because the studies are funded by the same companies selling you the overpriced substitute. They want you dependent on their products. Don’t be fooled. Eat real. Eat simple. Eat ancient. The body remembers.