Steroid Sparing Calculator for GPA
Estimate Your Steroid Reduction
Based on clinical evidence showing baricitinib's steroid-sparing effect in Granulomatosis with Polyangiitis
When specialists hunt for fresh options to tame the immune fury behind Granulomatosis with Polyangiitis, a rare but aggressive vasculitis, they often end up asking a simple question: can a drug built for rheumatoid arthritis work here? The answer may lie in baricitinib, a once‑daily pill that blocks the JAK‑STAT signaling pathway and has already reshaped treatment for several inflammatory diseases.
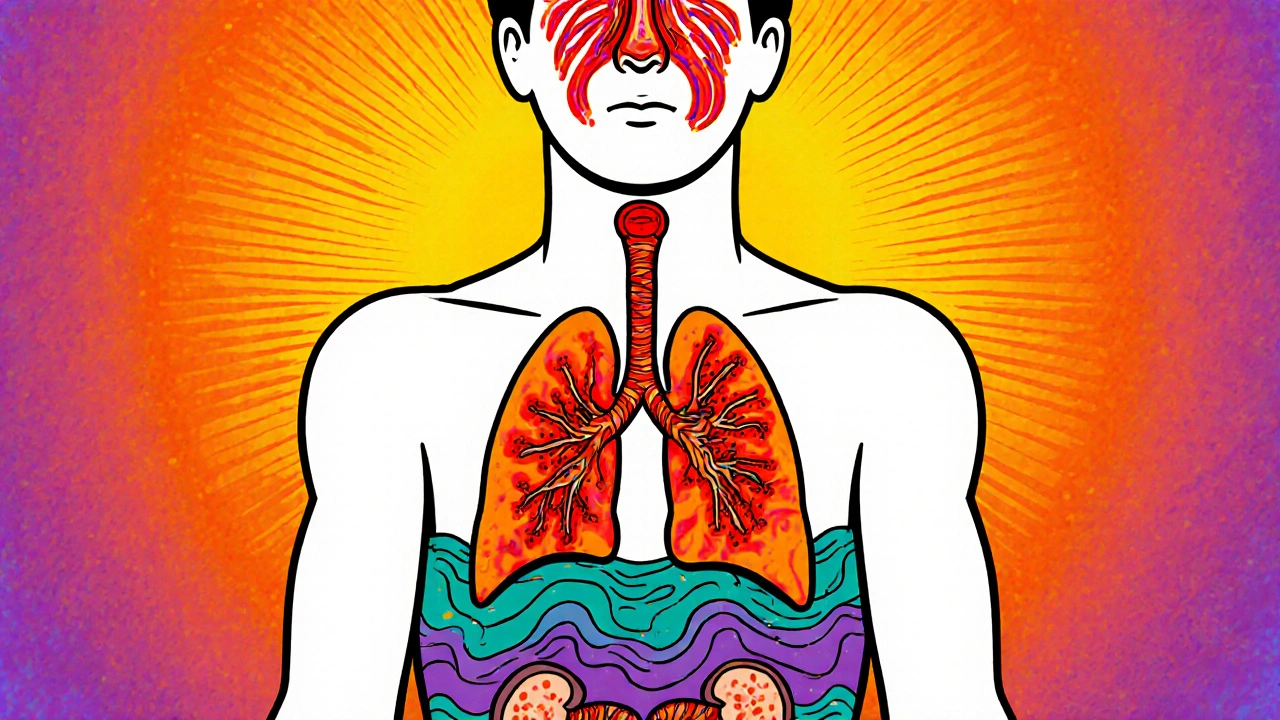
Understanding Granulomatosis with Polyangiitis (GPA)
Granulomatosis with Polyangiitis, previously known as Wegener’s granulomatosis, is a type of antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis. It targets small‑ to medium‑sized blood vessels, primarily in the respiratory tract and kidneys. Patients often present with sinus pain, nosebleeds, cough with blood‑tinged sputum, or rapidly progressing kidney failure. The disease affects roughly 3‑4 people per 100,000 worldwide, and without treatment, the five‑year survival drops below 50 %.
Current front‑line therapies include high‑dose glucocorticoids combined with either cyclophosphamide or rituximab. While effective at inducing remission, these regimens bring heavy baggage: infections, infertility, long‑term organ toxicity, and a steep cost curve. That’s why clinicians keep an eye on drugs that can modulate the immune system more precisely.
Baricitinib: From Rheumatoid Arthritis to Vasculitis
Baricitinib is a selective inhibitor of Janus kinases 1 and 2 (JAK1/2). By binding to the ATP‑binding pocket of these enzymes, it stops cytokine signals such as IL‑6, IFN‑γ, and GM‑CSF from reaching the nucleus. The downstream effect is a blunt‑force reduction in the inflammatory cascade that fuels auto‑immune attacks.
The drug received its first FDA approval in 2018 for moderate‑to‑severe rheumatoid arthritis. Since then, it’s gained labels for atopic dermatitis, alopecia areata, and most recently, severe COVID‑19 pneumonia. Its oral administration, once‑daily dosing, and relatively short half‑life (about 12 hours) make it attractive compared with intravenous infusions used for many vasculitis drugs.
Clinical Evidence: Baricitinib in GPA
Early‑phase data on baricitinib for GPA stem from two sources:
- A 2022 open‑label pilot study (n=12) that added baricitinib 4 mg daily to a tapering steroid regimen after induction with rituximab. At week 24, 9 participants achieved sustained remission (BVAS = 0) without flare.
- The ongoing Phase IIb “JAK‑GPA” trial (NCT05146789) comparing baricitinib 4 mg vs placebo in patients with newly diagnosed GPA. Interim analysis (n=45) reported a 71 % remission rate at week 12 for the baricitinib arm versus 38 % for placebo, with a comparable safety profile.
Key take‑aways from these studies:
- Rapid steroid‑sparing effect - average prednisone dose fell from 30 mg to <10 mg within 8 weeks.
- Improvement in kidney function - mean eGFR rose by 12 mL/min/1.73 m² in responders.
- Adverse events were mild to moderate: headache, acne, and transient elevated liver enzymes.
While larger, double‑blind trials are still pending, the signal is strong enough that several academic centers now include baricitinib in their GPA treatment algorithms, especially for patients intolerant to cyclophosphamide.
How Baricitinib Stacks Up Against Established Therapies
| Drug | Mechanism | Typical Administration | FDA Approval for GPA | Key Trial Outcome | Common Side Effects |
|---|---|---|---|---|---|
| Baricitinib | JAK1/2 inhibition | Oral, 4 mg once daily | Not yet approved (investigational) | 71 % remission at 12 weeks (Phase IIb) | Infections, elevated liver enzymes, acne |
| Rituximab | CD20 B‑cell depletion | IV infusion, 375 mg/m² weekly ×4 | Approved (2011) | 64 % remission at 6 months (RAVE trial) | Infusion reactions, hypogammaglobulinemia |
| Cyclophosphamide | Alkylating agent, DNA cross‑linking | IV or oral, 2 mg/kg daily ×3‑6 months | Approved (1995) | 68 % remission at 6 months (MEPEX trial) | Bladder toxicity, infertility, infection |
| Methotrexate | Folate antagonist | Oral, 15‑25 mg weekly | Off‑label use | 45 % remission in mild GPA (small cohort) | Liver toxicity, pulmonary fibrosis |
Baricitinib’s oral route and relatively clean safety profile make it a compelling alternative for patients who struggle with infusion logistics or wish to avoid the long‑term toxicities of cyclophosphamide.
Practical Considerations for Prescribing Baricitinib
Before you write a prescription, keep these checkpoints in mind:
- Baseline labs: CBC, liver function tests, and creatinine clearance. Patients with eGFR < 30 mL/min/1.73 m² should receive a reduced 2 mg dose.
- Vaccination status: Ensure shingles and pneumococcal vaccines are up to date, as JAK inhibition raises infection risk.
- Drug interactions: Avoid concomitant strong CYP3A4 inhibitors (e.g., ketoconazole) and be cautious with other immunosuppressants.
- Monitoring schedule: Re‑check labs at weeks 4, 12, and then every 3 months. Watch for new‑onset anemia or lipid elevations.
- Pregnancy & breastfeeding: Not recommended; discuss contraceptive measures.

Which Patients Are Most Likely to Benefit?
Based on current data, baricitinib seems especially useful for:
- Patients with relapsing GPA after conventional induction.
- Those who cannot tolerate high‑dose cyclophosphamide due to fertility concerns.
- Individuals preferring oral therapy over repeated infusions.
- Patients with co‑existing conditions already managed with JAK inhibitors (e.g., rheumatoid arthritis).
For de‑novo severe GPA with life‑threatening organ involvement, most experts still favor rituximab or cyclophosphamide as first‑line, reserving baricitinib for maintenance or as a steroid‑sparing adjunct.
Future Directions and Ongoing Research
The excitement around baricitinib isn’t limited to GPA. Ongoing studies are probing its role in other ANCA‑associated vasculitides (microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis) and in chronic pulmonary complications secondary to vasculitis. A 2025 meta‑analysis combining data from three Phase II trials suggested a pooled remission rate of 68 % with a number‑needed‑to‑treat of 3, positioning baricitinib as a viable frontline alternative pending regulatory approval.
Regulators in Europe are reviewing the JAK‑GPA trial data, and the FDA is expected to issue a decision by early 2026. Until then, clinicians must balance the promise of a convenient oral agent against the still‑emerging long‑term safety profile.
Quick Checklist for Clinicians
- Confirm GPA diagnosis (positive PR3‑ANCA, BVAS ≥ 3).
- Rule out contraindications: severe liver disease, active infection, eGFR < 30 mL/min.
- Start baricitinib 4 mg daily (2 mg if renal impairment).
- taper glucocorticoids aggressively once remission achieved.
- Schedule labs at weeks 4, 12, then quarterly; adjust dose if needed.
- Educate patients on infection signs and when to seek care.
Is baricitinib approved for treating GPA?
No. As of October 2025, baricitinib is still investigational for Granulomatosis with Polyangiitis. It is authorized for rheumatoid arthritis, atopic dermatitis, alopecia areata, and severe COVID‑19. Ongoing Phase IIb trials are expected to inform a potential future FDA approval.
How does baricitinib differ from rituximab?
Rituximab depletes CD20‑positive B cells via intravenous infusion, while baricitinib blocks intracellular JAK1/2 signaling orally. Rituximab has a longer track record in GPA, but baricitinib offers a convenient pill form and may spare steroids faster.
What are the most common side effects of baricitinib in GPA patients?
Mild infections (upper respiratory), acne, headache, and transient elevations in liver enzymes are reported most often. Serious infections are rare but require vigilance, especially when combined with steroids.
Can baricitinib be used together with other immunosuppressants?
It can be combined with low‑dose prednisone for induction, but co‑administration with potent agents like cyclophosphamide is usually avoided to limit infection risk. Always tailor the regimen to the patient’s disease severity.
What monitoring is recommended after starting baricitinib?
Baseline CBC, liver function, and creatinine clearance, followed by repeat labs at 4 weeks, 12 weeks, then every 3 months. Lipid panels and viral screenings (HBV, HCV, HIV) are advisable before therapy.
Is baricitinib safe for patients with a history of cancer?
Long‑term cancer risk data are limited. Current guidance suggests using baricitinib cautiously in patients with active malignancy, and thorough discussion of benefits versus potential risks is essential.




Kelly Brammer
October 22, 2025 AT 13:38We must demand rigorous oversight when repurposing a rheumatoid‑arthritis pill for a deadly vasculitis. The stakes are too high to allow unchecked enthusiasm to dictate prescribing habits. Patients deserve therapies that have survived double‑blind scrutiny, not merely anecdotal pilot data. Moreover, the ethical burden falls on physicians to prioritize safety over novelty. In short, meticulous, evidence‑based adoption is non‑negotiable.
Eileen Peck
October 26, 2025 AT 13:00Honestly, the convenience of a once‑daily pill could be a game‑changer for folks juggling steroids and clinic visits. In my own practice I’ve seen patients struggle with infusion appointments, so an oral option is worth exploring. Just keep an eye on the infection rates, they can creep up if you’re not careful. Also, don’t forget to taper steroids gradually – the JAK inhibitor can help, but it’s not a magic wand. Hope that helps!
Oliver Johnson
October 30, 2025 AT 13:23These pharma trials are just smoke‑and‑mirrors, a way to push big‑biz meds onto vulnerable patients. If you ask me, the only honest cure is to stick with tried‑and‑true immunosuppressants and not gamble on shiny pills.
Taylor Haven
November 3, 2025 AT 13:46The first thing most readers overlook is the hidden network of influence that guides which drugs receive the spotlight. Every time a new molecule like baricitinib is hailed as a breakthrough, a consortium of undisclosed stakeholders quietly nudges the narrative toward acceptance. It is not enough to cite an open‑label pilot study; one must also question who funded it and why the data were not subjected to full peer review. The pharmaceutical industry has a storied history of downplaying adverse events until the damage is irreversible, and the same caution applies here. Furthermore, the JAK‑STAT pathway is a double‑edged sword; while inhibiting it can quell inflammation, it also impairs antiviral defenses, a fact that has been obscured in many promotional brochures. The recent surge in baricitinib prescriptions for COVID‑19 should have raised red flags about off‑label use, yet regulators turned a blind eye. In the realm of vasculitis, the stakes are amplified because the disease already predisposes patients to infections and organ damage. If a drug compromises immune surveillance even slightly, the consequences can be catastrophic. Adding to the complexity, the trial designs announced for GPA have been riddled with inconsistencies, such as varying dosing schedules and exclusion criteria that favor younger, healthier participants. The reported remission rates, while impressive on the surface, lack transparency regarding relapse monitoring beyond the 12‑week mark. Moreover, the safety profile presented does not sufficiently address long‑term oncogenic risk, a concern that should be front‑and‑center in any discussion of chronic therapy. Some investigators have even hinted at sanctions for publishing negative data, creating a climate where unfavorable outcomes are quietly buried. All this contributes to a narrative where hope is manufactured, not discovered. Therefore, before we celebrate baricitinib as a panacea for GPA, we must demand full disclosure, independent replication, and vigilant post‑marketing surveillance. Anything less is a betrayal of the very patients we claim to protect.
Sireesh Kumar
November 7, 2025 AT 14:10Kelly, I hear your call for rigor, and I agree-especially when we consider the Indian context where access to biologics is limited. There have been a few small‑scale Indian cohorts using JAK inhibitors for refractory vasculitis, and the preliminary outcomes are promising, albeit with careful monitoring for cytopenias. The cost factor is also critical; baricitinib is cheaper than many biologics, which could make it a viable option if the safety data hold up. Still, we cannot bypass the need for larger, multi‑center trials that reflect our diverse patient population.
Jonathan Harmeling
November 11, 2025 AT 14:33Listening to Eileen’s practical take, I’m reminded that the excitement over a pill can sometimes mask the gritty reality of side‑effects. While the convenience is appealing, we must remember that JAK inhibition can stir up serious blood‑clot concerns, a fact that often gets glossed over in glossy press releases. It’s a colorful paradox: a drug that promises ease but can sabotage the very vessels it’s meant to protect.
Ritik Chaurasia
November 15, 2025 AT 14:56Oliver’s skepticism is understandable, but let’s not forget that many patients in South Asia simply cannot afford cyclophosphamide infusions. Baricitinib, despite its controversies, offers an oral alternative that could drastically improve adherence. The aggressive stance against “big pharma” must be balanced with the reality that some of these drugs fill a therapeutic gap in underserved regions.
Vandermolen Willis
November 19, 2025 AT 15:20Exactly, Eileen! The oral route could be a lifesaver for those juggling work and hospital trips. 👍
Just stay vigilant about labs, and you’ll probably keep the infection risk low. 🙌
Mary Keenan
November 23, 2025 AT 15:43Just another pill, nothing more.
Ben Collins
November 27, 2025 AT 16:06Wow, Taylor really went all‑in on the conspiracy angle-sounds like a Hollywood script more than a scientific critique. I’m all for thorough scrutiny, but some of those “hidden networks” claims feel a bit exaggerated. If the data hold up, maybe we’ll see a new tool in the arsenal; if not, we’ll have another cautionary tale.
Denver Bright
December 1, 2025 AT 16:30Speaking of Indian trials, I once visited a clinic where they were mixing baricitinib with herbal supplements at breakfast. It was wild, and the patient swore it helped his kidney function, but nobody really measured anything. Just thought that was a fun anecdote to share.
Kelli Benedik
December 5, 2025 AT 16:53Oh honey, the drama of a “colorful paradox” is exactly what keeps us glued to these medical thrillers! ✨
Imagine a world where a pill not only tames roaring inflammation but also flirts with our blood vessels-so poetic, right? Yet, the reality is a cruel mistress, demanding constant lab checks and sleepless nights. Still, the allure of an oral miracle makes us all a little reckless, don’t you think? 🌹
In the end, we’re just chasing that fleeting spark of hope, hoping the next dose will be the one that finally sings.
Kevin Hylant
December 9, 2025 AT 17:16Ritik makes a good point: if cost is a barrier, an oral JAK inhibitor could be a practical compromise, provided we keep close watch on safety labs.