A cerebral aneurysm isn’t something you hear about until it’s too late. Most people never know they have one - until it bursts. About 3.2% of adults worldwide carry an unruptured brain aneurysm, but only a small fraction will ever experience a rupture. Still, when it happens, the chances of dying within the first day are between 30% and 40%. That’s why understanding cerebral aneurysm risk factors and treatment options isn’t just medical knowledge - it’s life-saving awareness.
What Makes a Cerebral Aneurysm Likely to Burst?
A brain aneurysm is a weak spot in a blood vessel that balloons out like a blister. Not all of them rupture. But some are ticking time bombs. The biggest red flag is size. If an aneurysm is 7 millimeters or larger, your risk of rupture jumps by more than three times compared to smaller ones. Shape matters too. Irregular, lobed aneurysms - especially those with smaller bulges called daughter sacs - are nearly three times more likely to burst than smooth, round ones.
Location plays a huge role. Aneurysms near the front of the brain, especially at the anterior communicating artery (AComm), rupture far more often than others - even when they’re under 5 mm. In fact, AComm aneurysms are 2.4 times more likely to rupture than those in other spots. And distal anterior cerebral artery aneurysms? They can burst at sizes most doctors would consider safe.
Then there’s blood flow. Research using computer models shows that areas with chaotic, low, or back-and-forth blood flow - called oscillatory wall shear stress - are where 83% of ruptured aneurysms form. It’s not just about size. It’s about how blood pushes and pulls on the vessel wall over time.
Who’s Most at Risk?
Some risks you can’t change. Age is one. After 65, your rupture risk more than doubles. Women are 1.6 times more likely than men to develop aneurysms. And if two or more close family members had one, your risk quadruples. Genetics matter - studies have found 17 specific gene locations linked to aneurysm formation and rupture.
But many risks are within your control. High blood pressure is the biggest modifiable danger. If your systolic pressure is above 140 mmHg, your rupture risk shoots up by 2.3 times. Smoking is even worse. Current smokers face a 3.1-fold higher risk. And it’s not just whether you smoke - it’s how much. People who smoke 10 or more cigarettes a day see their risk climb by 47%. Quitting cuts that risk by 54% within two years.
Heavy drinking also adds danger. More than 14 drinks a week increases rupture risk by 32%. Combine smoking, high blood pressure, and heavy drinking, and you’re stacking the odds against you.
Having more than one aneurysm? Your rupture risk jumps nearly fourfold. And if you’ve already had one rupture, your chance of another is more than five times higher. That’s why follow-up scans are critical after any rupture event.
The PHASES Score: A Real-World Tool for Deciding What to Do
Doctors don’t guess whether to treat or watch. They use tools. The most trusted is the PHASES score. It combines six factors: your population background, blood pressure, age, aneurysm size, whether you’ve had a previous bleed, and the aneurysm’s location. Each factor adds points. A score of 0-3 means your five-year rupture risk is only 3%. A score of 9-10? That’s 45%.
Every single point increase raises your risk by 32%. So if you’re at a PHASES score of 6 or higher, most specialists recommend treatment. Below 6? Monitoring with yearly MRA scans is often the better path - especially for small aneurysms in low-risk areas.
There’s also the ELAPSS score (for one-year risk) and the triple-S model (size, site, shape), which predicts rupture chances within six months to two years with good accuracy. These aren’t just academic tools. They’re used daily in hospitals across the UK and US to decide who needs surgery and who can wait.
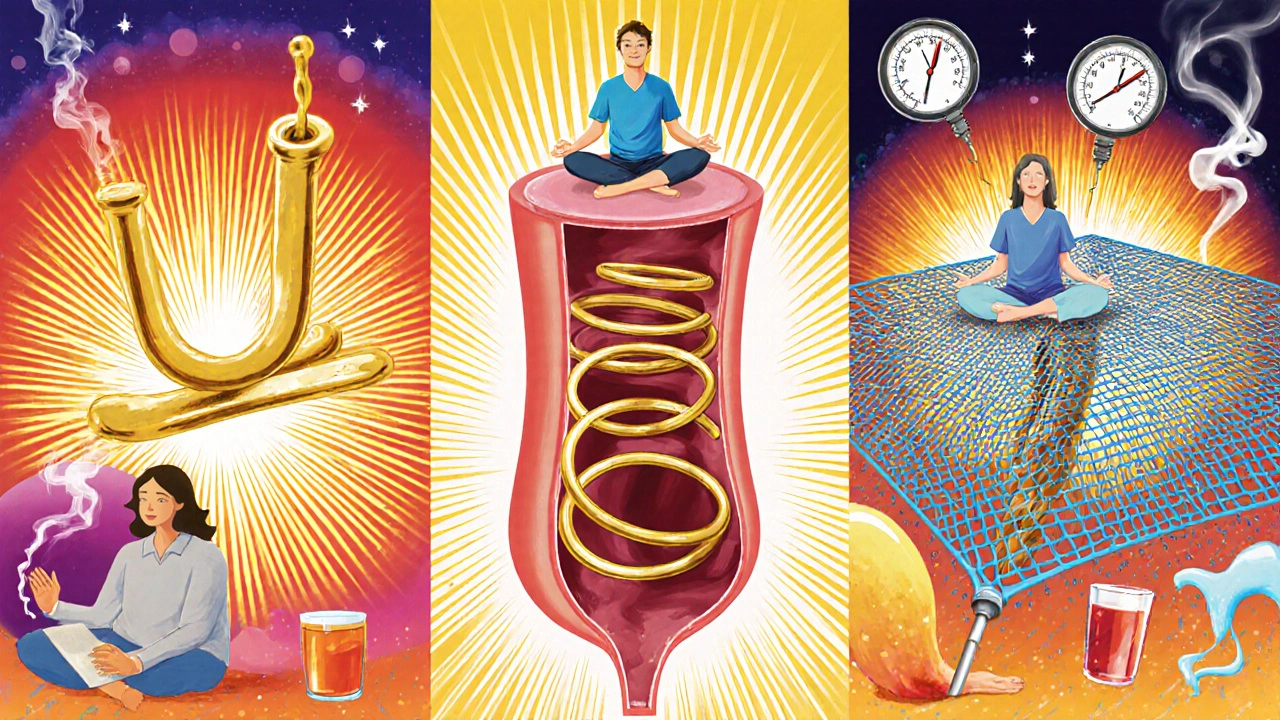
Treatment Options: Clipping, Coiling, and Flow Diversion
If treatment is needed, there are three main approaches. Each has pros, cons, and ideal candidates.
Surgical clipping is the oldest method, dating back to 1937. A neurosurgeon opens the skull, finds the aneurysm, and clamps it shut with a tiny titanium clip. It’s a one-time fix - 95% of clipped aneurysms are fully sealed. Long-term, 88-92% stay closed forever. But it’s invasive. Recovery takes weeks. Complication rates: 4.7% permanent disability, 1.5% death.
Endovascular coiling is less invasive. A catheter is threaded from the groin up to the brain. Platinum coils are packed into the aneurysm, triggering a clot that seals it off. Success rate at six months: 78-85%. It’s faster, less painful, and patients go home sooner. But it’s not always permanent. About 16% of coiled aneurysms need retreatment within 12 years. Morbidity is lower than clipping - 3.9% - and mortality is just 1.1%.
Flow diversion is the newest option. It uses a mesh stent - like the Pipeline Embolization Device - placed across the aneurysm neck. Blood flows through the mesh, away from the bulge, and the aneurysm slowly shrinks and seals. It’s especially good for large, wide-necked, or complex aneurysms. At one year, 85.5% of treated aneurysms are fully closed. But it takes time - the healing process can last months. Complication rates are slightly higher than coiling (5.2% morbidity), but death risk is the lowest of the three: just 0.8%.
For aneurysms at the base of the brain - like those in the middle cerebral artery - clipping has a higher complication rate. That’s why many centers now prefer flow diversion or coiling for posterior circulation cases.
What About Newer Devices Like the WEB?
Yes, there’s more. The Woven EndoBridge (WEB) device is FDA-approved for aneurysms that split into two branches - called bifurcation aneurysms. It’s a small, cage-like device that sits inside the aneurysm, blocking blood flow without needing to coil or divert. In trials, 71.4% of treated aneurysms were fully closed after one year. It’s not for everyone, but for the right patient, it’s a game-changer.
What Happens If You Don’t Treat It?
Many small, low-risk aneurysms are left alone. The UCAS Japan study found that aneurysms under 5 mm in the front of the brain had only a 0.2% chance of rupturing over five years. Even those in the back of the brain - a higher-risk zone - had just a 0.7% risk. That’s lower than the risk of a car accident on your daily commute.
But monitoring is non-negotiable. Annual MRA scans catch growth early. If an aneurysm grows by even 1 mm, your risk spikes. That’s why follow-up isn’t optional. It’s essential.
Medical Management: The Silent Protector
Treatment isn’t just about surgery or coils. The most powerful tool many patients have is medication and lifestyle change. Strict blood pressure control - keeping it under 130/80 - is the single most effective way to reduce rupture risk. Smoking cessation alone cuts risk by over half. Cutting back on alcohol helps too.
No drug can make an aneurysm disappear. But controlling these factors can stop it from growing or bursting. For many, this is the best option - especially if their PHASES score is low.
Long-Term Outcomes: Life After Treatment
Successful treatment cuts the 10-year re-rupture risk from 68% down to just 2.3%. That’s a massive difference. But recovery isn’t just about survival. Quality of life matters.
Patients who undergo endovascular treatment report higher quality of life scores at one year than those who have surgery. The EQ-5D scale - which measures mobility, self-care, pain, and daily function - shows scores of 0.82 for coiling versus 0.76 for clipping. That gap might seem small, but in real life, it means returning to work sooner, needing less help at home, and feeling more like yourself.
What’s Next? The Future of Prediction and Treatment
Researchers aren’t stopping. Machine learning models are now analyzing 42 different features - shape, flow patterns, wall thickness - to predict rupture better than any score system can. Genetic testing is becoming more precise. The HUNT study in Norway identified specific gene variants that make some people far more vulnerable.
Soon, we may be able to look at a scan and say: “This aneurysm has a 9% chance of bursting in the next year.” Not “maybe,” not “possibly.” A number. That’s the future. And it’s closer than you think.
Can a cerebral aneurysm go away on its own?
No, a cerebral aneurysm won’t disappear without treatment. Once it forms, it stays unless it’s sealed off by surgery, coiling, or flow diversion. In rare cases, a small aneurysm may clot off naturally, but this is unpredictable and not something to rely on. Monitoring is essential - even if you feel fine.
How often should I get scanned if I have an unruptured aneurysm?
Annual MRA (magnetic resonance angiography) scans are the standard for unruptured aneurysms. If your aneurysm is small, stable, and your PHASES score is low, yearly scans are usually enough. If it’s growing, larger than 7 mm, or you have other risk factors, your doctor may recommend scans every 6 months. Never skip follow-ups - growth often happens without symptoms.
Is coiling better than clipping?
It depends. Coiling is less invasive, has lower short-term mortality, and allows faster recovery - making it better for older patients or those with other health issues. Clipping offers a more permanent solution with lower retreatment rates. For complex or wide-necked aneurysms, flow diversion may be better than either. The decision isn’t one-size-fits-all. It’s based on size, location, your age, and overall health.
Can I exercise with a cerebral aneurysm?
Yes - but carefully. Light to moderate exercise like walking, swimming, or cycling is safe and even encouraged. Avoid heavy lifting, intense weight training, or activities that cause sudden spikes in blood pressure. If you’re unsure, talk to your neurologist. A stress test or blood pressure monitoring during activity can help guide what’s safe for you.
What are the signs a cerebral aneurysm is about to rupture?
Most unruptured aneurysms cause no symptoms. But a sudden, severe headache - often described as the “worst headache of your life” - is the classic warning sign. Other red flags include double vision, drooping eyelid, nausea, vomiting, stiff neck, or loss of consciousness. If you experience any of these, call emergency services immediately. Time is critical.
Does having a family history mean I’ll definitely get one?
No. Having a family history increases your risk - especially if two or more close relatives had one - but it doesn’t guarantee you’ll develop one. About 1 in 30 people with a family history will have an aneurysm. Screening with MRA is recommended for those with two or more affected relatives. Early detection saves lives.
What Should You Do Now?
If you’ve been told you have an unruptured aneurysm, don’t panic. Most won’t rupture. But don’t ignore it either. Get your PHASES score. Know your aneurysm’s size, shape, and location. Quit smoking. Control your blood pressure. Stick to your scan schedule. Talk to your neurologist about whether treatment makes sense for you - not just because it’s possible, but because it’s right for your life.
For everyone else: know the signs. Know your family history. And if you ever feel that sudden, unbearable headache - don’t wait. Get help immediately. It could be the difference between life and death.



Ashley Unknown
November 16, 2025 AT 13:26Okay but have you ever heard of the secret government program that plants aneurysms in people’s brains to control population growth? I know a guy whose cousin’s neighbor got diagnosed after she stopped drinking kombucha - they said it was ‘natural’ but the MRI showed weird metallic flecks. They’re not telling us the truth. I’ve been researching this for 3 years. The WHO is in on it. They use 5G towers to trigger rupture in high-risk zones. I’m not crazy, I have spreadsheets. 🤫
Georgia Green
November 17, 2025 AT 06:05Just wanted to say thanks for this post - super helpful. I had a 4mm aneurysm found on accident during a migraine scan last year. My doc said PHASES score was 2, so we’re doing yearly MRA. Quit smoking 6 months ago and my BP’s been under 120/80. Feels good to take control. One typo: ‘distal anterior cerebral artery’ - I think you meant ‘distal anterior communicating artery’? Not sure though, double check? 😊
Christina Abellar
November 17, 2025 AT 15:14This is exactly the kind of clear, calm info we need. No panic, just facts. Thanks for sharing.
Eva Vega
November 17, 2025 AT 21:50The hemodynamic parameters referenced - specifically oscillatory wall shear stress (OWSS) - are indeed critical predictors of rupture susceptibility, as validated by computational fluid dynamics (CFD) modeling in the 2022 JNS study. The aneurysm’s geometric complexity, particularly the presence of daughter sacs, correlates with elevated vorticity and low Reynolds number zones, which promote endothelial dysfunction. For clinical application, the ELAPSS model offers superior temporal resolution for 12-month risk stratification compared to PHASES, especially in posterior circulation lesions.
Matt Wells
November 19, 2025 AT 12:41While the article presents a reasonably comprehensive overview, it fails to adequately address the limitations of the PHASES score in pediatric populations. Furthermore, the omission of the 2023 meta-analysis by the International Society for Cerebrovascular Disease, which demonstrates a 17% underestimation of rupture risk in women under 55, is a significant scholarly oversight. One must question the editorial rigor of such a piece disseminated to the general public.
Margo Utomo
November 20, 2025 AT 18:30Y’all are doing SO GOOD. 🙌 I had a coiled aneurysm in 2021 - no regrets. Went back to yoga in 3 weeks. My neurologist said I’m basically a superhero now. 💪 Quit smoking. Drink water. Sleep. You got this. And if your doc says ‘watch and wait’ - trust them. But also, get a second opinion. And a therapist. 😅❤️
George Gaitara
November 22, 2025 AT 03:13This whole post feels like a pharmaceutical sales pitch. Coiling? Flow diversion? Please. They’re just selling expensive gadgets to avoid doing real surgery. I’ve seen too many people get ‘minimally invasive’ treatments that fail in 2 years and then they need open craniotomy anyway. And why is no one talking about how insurance companies push these procedures? It’s all profit. Wake up.
Deepali Singh
November 22, 2025 AT 08:50Statistically, the probability of rupture for aneurysms under 5mm in the anterior circulation is 0.2% per year. But that’s an aggregate. The variance within subpopulations - particularly in hypertensive smokers over 60 - exceeds 12x the baseline. Your article conflates population-level risk with individual vulnerability. You’re not providing insight. You’re providing false reassurance.
Sylvia Clarke
November 23, 2025 AT 23:55Interesting how we’ve gone from ‘wait and see’ to ‘predict and prevent’ - and yet, we still treat patients like data points. The PHASES score is a tool, not a verdict. What about the woman who’s terrified of hospitals but lives 200 miles from a neuro center? Or the man who can’t afford to take time off work for scans? Medicine needs to stop pretending risk calculators are the whole story. Sometimes, the most life-saving thing isn’t a clip or a coil - it’s compassion.
Jennifer Howard
November 25, 2025 AT 14:02It is imperative that individuals who have been informed of the presence of an unruptured cerebral aneurysm immediately cease all forms of physical exertion, discontinue consumption of all beverages containing caffeine, and submit to mandatory psychiatric evaluation - for the emotional instability associated with such a diagnosis may itself precipitate a rupture. Furthermore, one must consider the moral obligation to disclose this condition to all romantic partners, as failure to do so constitutes a form of bioethical malfeasance. This is not a medical issue - it is a moral imperative.