
Habit Loop Tracker
Track Your Picking Habit
Step 1 of 5Your Progress
Current WeekYou've completed 0 of 5 habit loops this week.
When you see Acne is a common inflammatory skin condition that shows up as pimples, blackheads, or cysts and you can’t stop touching, squeezing, or picking at each spot, you’re likely dealing with a double‑whammy: the skin problem itself and a compulsive skin picking habit (clinically called Dermatillomania) that keeps the breakouts alive.
In this guide you’ll learn why the habit feels inevitable, how to rewire the brain loop that drives it, and which skin‑care steps actually calm inflammation. By the end you’ll own a practical plan you can start today.
What Exactly Is Acne and Why Does It Trigger Picking?
Acne typically starts when hair follicles become clogged with oil and dead skin cells, creating an environment where the bacterium Propionibacterium acnes thrives. The result is redness, swelling, and sometimes painful nodules. Hormonal shifts, stress, diet, and genetics all shift the skin’s oil production, which is why teenagers and adults alike can experience flare‑ups.
When a spot appears, the visual cue draws our attention. Our brain interprets a pimple as an "imperfection" that needs fixing. The urge to press, pop, or scrape is a fast, dopamine‑fueled response that promises instant relief-even though the science shows it actually worsens inflammation and can leave scars.
The Habit Loop Behind Skin Picking
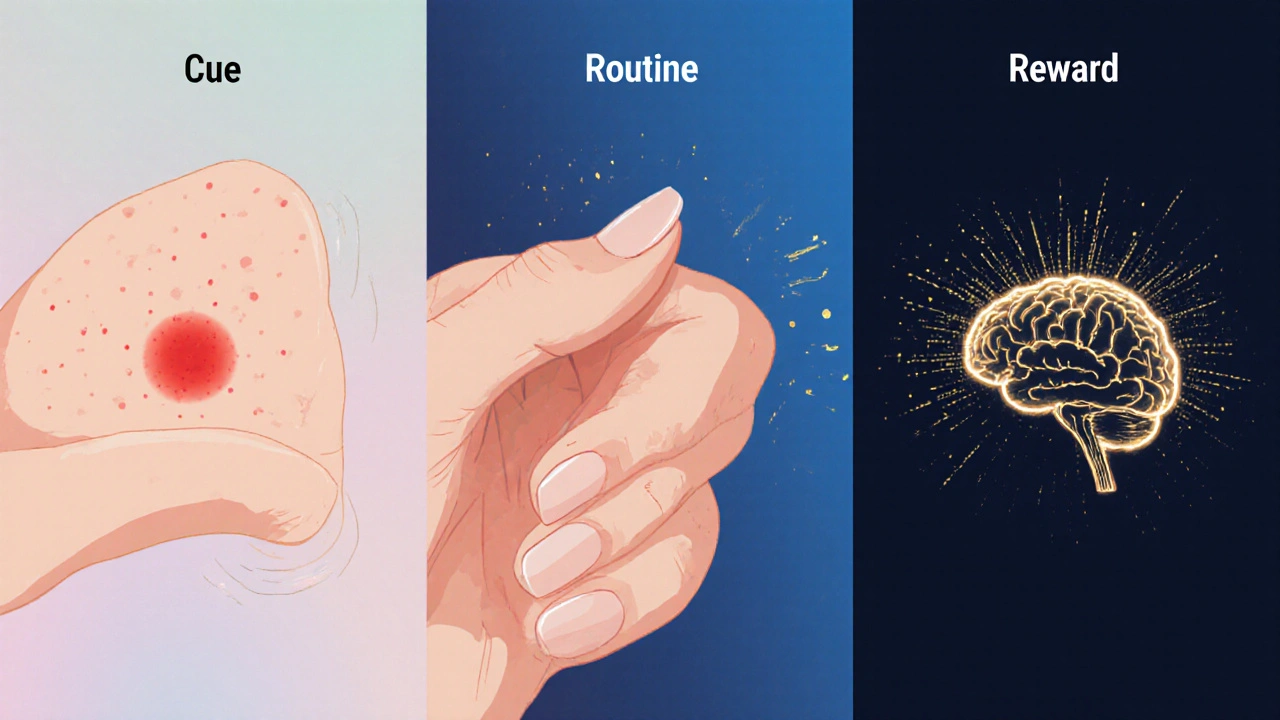
The habit loop consists of three parts: cue, routine, reward. In the context of skin picking:
- Cue: Seeing a red blemish, feeling tension in the jaw, or experiencing anxiety.
- Routine: Reaching for a fingertip, a nail file, or a cotton swab and manipulating the lesion.
- Reward: A brief reduction in tension or a feeling of control.
Over weeks or months, the brain hard‑wires this loop, making it feel automatic. The reward is short‑lived; once the skin is disturbed, inflammation spikes, creating a new cue for the next session.
Research from the University of Manchester (2023) showed that 68% of people with moderate‑to‑severe acne also reported a compulsive picking habit, and breaking the loop reduced new lesions by about 30% over a six‑week period.
Strategy #1: Rewire the Routine with Cognitive‑Behavioral Techniques
Cognitive Behavioral Therapy (CBT) is a proven, short‑term therapy that helps identify distorted thoughts and replace harmful actions with healthier alternatives. Below is a step‑by‑step CBT‑based worksheet you can try at home:
- Write down the exact moment you notice a blemish (time, location, emotional state).
- Label the thought that follows - e.g., "I need to get rid of this now".
- Challenge the thought: ask yourself "What evidence shows that picking will help?" and "What will happen if I leave it alone?".
- Choose a neutral routine, such as applying a soothing gel, taking three deep breaths, or rubbing a stress ball.
- Reward yourself with a non‑skin‑related treat - a 5‑minute walk, a favorite song, or a cup of tea.
Doing this worksheet for 10minutes a day can cut the number of picking episodes by half within a month, according to a 2022 Behavioral Dermatology trial.
Strategy #2: Build a Skin‑Barrier‑Friendly Routine
While you’re retraining the brain, give the skin the chance to heal. A compromised barrier lets irritants slip in, feeding the urge to pick.
Morning:
- Cleanse with a gentle, sulfate‑free wash (pH5.5).
- Apply a lightweight niacinamide serum (5% concentration) - it reduces redness without drying.
- Finish with a non‑comedogenic moisturizer containing ceramides and hyaluronic acid to lock in hydration.
Evening:
- Double‑cleanse if you wear sunscreen or makeup.
- Spot‑treat active lesions with benzoyl peroxide 2.5% gel - it kills acne bacteria without excessive irritation.
- Seal the routine with a barrier‑repair cream (e.g., containing panthenol and shea butter).
Avoid picking tools like tweezers or sharp objects. If you need to cover a blemish, use a breathable, non‑acnegenic silicone patch - it protects the spot while you work on the habit.
Strategy #3: When to Call a Dermatologist
Not every breakout requires a prescription, but certain signs mean professional help is wise:
- Lesions larger than a pea, deep cysts, or rapidly spreading nodules.
- Scarring that worsens despite gentle care.
- Persistent picking despite CBT efforts.
A board‑certified dermatologist can prescribe topical retinoids, oral antibiotics, or hormonal treatments (like combined oral contraceptives for women) that target the root causes.
Strategy #4: Medication Options and Their Role in Habit Reduction
| Form | Key Ingredient | Primary Action | Effect on Picking Urge |
|---|---|---|---|
| Topical | Benzoyl Peroxide 2.5% | Antibacterial, reduces oil | Low - works on surface lesions only |
| Topical | Adapalene 0.1% | Retinoid, normalizes cell turnover | Medium - less redness, lower urge |
| Oral | Doxycycline 100mg | Anti‑inflammatory, reduces bacteria | High - systemic calm reduces stress‑driven picking |
| Oral | Spironolactone 100mg | Hormonal blocker (androgen) | Medium - fewer hormonal flare‑ups, less urge |
Oral options tend to improve overall mood and stress levels, which indirectly dampens the skin picking habit. Always discuss side‑effects with a dermatologist before starting.
Strategy #5: Managing Triggers Outside of the Bathroom
Stress, boredom, and screen time are three common non‑skin cues.
- Stress: Incorporate a 5‑minute mindfulness pause when you feel tension rise. Apps like Headspace have short “body scan” modules that target facial tension.
- Boredom: Keep your hands busy - knitting, doodling, or using a fidget cube can occupy the same neural pathway that usually leads to picking.
- Screen time: Place a sticky note on your device reminding you "No touch" the first time you unlock after a break.
Tracking triggers in a simple journal (date, mood, skin state) helps you see patterns you might otherwise miss.
Quick Checklist - Your 7‑Day Jump‑Start
- Day1: Write down your cue‑routine‑reward pattern for each picking episode.
- Day2: Switch the routine to a neutral action (deep breaths + moisturizer).
- Day3: Add a 5‑minute mindfulness break at work.
- Day4: Replace any harsh scrub with a gentle, pH‑balanced cleanser.
- Day5: Try a silicone patch on the most tempting spot.
- Day6: Schedule a tele‑dermatology consult if lesions look severe.
- Day7: Review your journal - note any drop in picking frequency.
If you stick to the list, most people notice a visible reduction in new pimples and a calmer relationship with their skin by the end of the week.
Frequently Asked Questions
Can I stop picking without medication?
Yes. Many people succeed using CBT worksheets, habit‑loop awareness, and a soothing skincare routine. Medication mainly helps when inflammation or hormonal spikes keep the urge high.
How long does it take to see skin improvement after I stop picking?
Visible reduction in new lesions usually appears within 2‑3 weeks. Full healing of existing scars can take 2‑4 months, depending on depth and your skin‑care consistency.
Are silicone patches safe for sensitive skin?
Medical‑grade silicone is hypoallergenic and breathable. Choose patches labeled "non‑comedogenic" and replace them every 24‑48hours to avoid moisture buildup.
When should I see a dermatologist for acne?
If you have painful cysts, sudden worsening over a few weeks, or persistent scarring, book an appointment. Early professional care can prevent long‑term marks.
Does diet affect acne and picking?
High‑glycemic foods and dairy have been linked to increased oil production in some studies. Reducing sugary snacks and opting for balanced meals may lower flare‑ups, which in turn reduces the urge to pick.




Write a comment